Endometriosis Foundation of America
Virtual Patient Conference, October 16-18, 2020
Endometriosis After Hysterectomy - Dr. Rosanne Kho
Margaret Caspler Cianci:
Next we are delighted to welcome Dr. Rosanne Kho to speak about endometriosis after hysterectomy. Dr. Kho is an obstetrician gynecologist in Cleveland, Ohio, and is affiliated with the Cleveland Clinic. She received her medical degree from Tulane and has been in practice for more than 20 years. Dr. Kho, welcome. We are delighted to have you with us today. Thank you so much on this important topic.
Rosanne Kho:
The privilege is mine, Margaret. Thank you for bringing this whole panel together and thank you Dr. Seckin for including me and thinking of me. I'm going to go ahead and start sharing my screen so Dr. Seckin asked me to talk about endometriosis after hysterectomy. And this is a wonderful topic, a topic that is very near and dear to my heart. What I would like to do when patients come for their care for endometriosis, the decision to make, to have a hysterectomy is a major one. So, but one thing that we all need to be aware of would be to have a really good discussion about what are the possibilities after having had a hysterectomy. And what do we talk about when we say hysterectomy? It is the removal of the uterus. I would like to share with you a couple of my patients here, whom I have seen recently.
I have seen recently with interesting situations or conditions, and this is after they have had their hysterectomies. This patient that I... The first one that I would like to share with you is one that I saw about two months ago. She's 49, came to me during the first quarter of this year. She presents with monthly bleeding. In 2015 she had a hysterectomy that was done laparoscopically and her left ovary was removed. So having said that, you now know that she still has her right ovary, and she's coming to me with monthly bleeding. She has severe pain with intercourse, chest pain with bowel movements, and she has pain on a daily basis. It should be mentioned that she has gone back to her primary surgeon who did her initial surgery. She has gone to two other surgeons after that visit as well. And they all pretty much said it must be dryness.
It must be something else, an infection that's causing this bleeding. So with her exam at the time that she came to me, I noticed that there was just a slight puckering, right at the top of the vaginal vault where her hysterectomy incision was. It was extremely tender to her as well. We did an MRI that was targeted for endometriosis. So at our center at the Cleveland clinic, our imaging modality is that of MRI. In some centers this can be done with a targeted transvaginal ultrasound, but at ours we use MRI. We have a protocol specifically for endometriosis, and unfortunately my mouse is not working here, but I wanted to show you that she has a lesion at the top of her vagina towards the right side.
So let's pause now and just think about her. I want to share with you another patient. This other patient is much younger. She's 40. She's had one vaginal delivery prior to coming to see me. And she comes in complaining of sharp, stabbing, pelvic pain on a daily basis. She has a history of stage four endometriosis. And this busy slide shows you that she's had at least five other hysterectomies prior to 2009, during which time she had an abdominal hysterectomy for endometriosis and ovarian cysts. Subsequent to that, so remind you now, at 33 years of age underwent an abdominal hysterectomy. At 35, she had both ovaries removed because she continued to have severe pain. She underwent three more surgeries after both ovaries were removed after her hysterectomy for continued pain and endometriosis.
She underwent an expensive peritectomy. That's the excision of the lining of the pelvic cavity. Also because an ovarian remnant tissue, and I'll talk to you in a little bit about this, was diagnosed her last surgery in 2016, actually the pathology no longer showed that there was ovarian tissue that was noted. When she came to see me, she still had significant pain.
So her pain was present five to six times per day. She was unable to maintain a job. She was unable to provide for her family. At the time that she came to see me. She was not on hormone replacement therapy for at least four months, but note that at 40 years of age, without hormone replacement therapy, she also didn't have hot flashes. You would expect someone who's had both ovaries removed, not on hormone replacement therapy, to have menopausal symptoms. What was interesting is that her FSH level, which is a hormone that we check, came back showing that she must be in menopausal range, but her estradiol was still elevated for a woman who's had both ovaries removed.
Again, we did a targeted MRI and that showed that there was some tissue on the left side of the pelvis sitting right on top of the vagina that was suspicious for ovarian looking tissue. And indeed that's what we ended up finding at the time of her surgery. So just in the next few minutes, what I would like to talk about is to just go over very briefly, a review of what surgical procedures are available for the primary diagnosis of endometriosis. What happens? What is the re operation rate after a hysterectomy?
We need to be very aware. As physicians who treat patients with endometriosis, we have to be aware of the possibility of residual or recurrent endometriosis, if not ovarian remanent tissue or the presence of ovarian tissue that can then stimulate the endometriotic cells. So just to go back and review, what are the primary surgical options for endometriosis? We think of there as being three primary options for surgery. That of a conservative approach, which means that the uterus is spared and the ovaries are left intact. This is advantageous for women who want to preserve fertility and the ability to have future pregnancies and also to preserve ovarian function.
Studies will show that compared to just a diagnostic laparoscopy where nothing else was done for the endometriosis, there's a significant reduction in the pain of these patients that of 73% compared to only 21% in patients who just went in for diagnostic laparoscopy. And just to mention, the 21% is pretty much a placebo effect. Patients who undergo conservative surgery have increased live birth and pregnancy rates as well compared to those with just a diagnostic laparoscopy. So let's move on now to a hysterectomy. So a hysterectomy is the removal of the uterus itself, right? When would we offer patients to undergo hysterectomy? When patients have persistent pain after having had a previous surgery. If medications no longer provide them with relief, and if they no longer are interested in future childbirth. After a shared decision-making a hysterectomy may be performed. And that is with the benefit of preserving ovarian function as well. Studies will show that this can be quite effective in reducing pain.
How about hysterectomy with the removal of the ovaries? That is pretty much taking the uterus and taking both ovaries out, putting the patient then into early menopause, what we call surgical menopause. The landmark study that is often cited is this one by Dr. Falcone, who was my previous chair here at the Cleveland clinic, who has now gone on to be the Chief of Staff at Cleveland clinic in London. And this is a good one for all of us to understand. So if we look at the re operation rate of patients who undergo all of these different types of surgeries, and what's nice about this study is that these patients were followed for up to seven years, of all of these surgeries. So laparoscopy alone, with both ovaries being preserved, in seven years up to 40% of these patients will require a re operation primarily for pain or for recurrence of the disease. With the hysterectomy, whether one or both ovaries are removed, there's up to a 22 to 24% chance of patients going through another procedure after their hysterectomy. And if the patient were to undergo hysterectomy and both ovaries removed, up to 8% required, another re operation. So again, a hysterectomy and having both ovaries removed, there still is a small percent of patients who would require another surgery. So it's not 0%, it's up to 8%. It's not frequent, but it's definitely there. And looking at this group of patients, what are the risk factors for re operation? Patients who are younger tend to have a greater risk for another surgery in the future. Incomplete excision at the time of their surgery also subjects them for a greater risk for another surgery in the future. Not being on medical therapy after their surgery, depending on what their first surgery was performed and whether or not there was residual disease also can place them at a higher risk for another procedure in the future. So let's go back now to our first patient right? Our first patient ended up with endometriosis that was found at the top of the vagina and also involving the rectum. Fortunately, the bowel wall was not completely involved. There was no nodule that was penetrating through the bowel, but she had significant fibrosis or what we call scarring that extended pretty much all the way down to the pelvic floor. Her left ureter was actually entrapped with fibrosis and scarring from the endometriosis. She ended up with an excision of all of the adhesions. We did a vaginectomy as well, which pretty much was to excise that small nodule up at the top of the vagina so that that could be excised completely. And the vaginal edges placed back together.
How about our second patient? Our second patient who had, just to recall, the patient who had undergone multiple previous other surgeries for ovarian remnant syndrome. Indeed, when we went back in, she had a nodule that was consistent with ovarian tissue. It was on the left pelvic sidewall. It was sitting right on top of the vagina as well. The bladder as well was actually involved. And so I had to take that lesion out and then put the bladder back together as well as the top of the vagina back together. So we don't need to go through the video, but just to show you the extent of the scarring that was involved, the left ureter was also involved.
So three months after her surgery, when she came back to me, her estrogen level had dropped. And for most women, while we don't really want to have no estrogen in our system, for her it was a relief. So finally she was free from pain. She was happy to mention to me, I now have hot flashes. Can I be started on estrogen replacement therapy? And that's indeed what we did was just to put her on a small amount so that she could be relieved from her hot flashes and could sleep better at night. So ovarian remnant syndrome as well studied, this is the landmark study that we published way back in the two thousands. I also put together a review paper, looking at ovarian remnant syndrome and the impact of endometriosis on this disease. This is an elder patient in her seventies who was found to have a residual ovarian tissue on her right side.
We found that there was a small portion of these women with ovarian remnant syndrome who ended up actually having ovarian cancer as well. So this is the up-to-date reference that I just recently updated in September of 2020 summarizing the findings of ovarian remnant syndrome. So some take home messages, right? Endometriosis can certainly be present if not recur, after a hysterectomy alone. It can recur or be present as well even when the ovaries have been removed. I think I echo strongly what Margaret said very early on at the start of this webinar, which is that I urge you as the patient to be your best advocate. You cannot give up in patients or in physicians who do not see many endometriosis patients. It's often dismissed, the findings, or the presentation of continued pain after hysterectomy can be dismissed, unless the physician has a high index of suspicion.
And this is what I strongly emphasize when I go around and give these talks and lectures. And the physician needs to perform a good history, understand the story, understand what the patient is going through and perform a very good physical exam. I do also believe in the important role of targeted imaging. So there are many centers now in the country that have targeted imaging just for endometriosis, and this should be done prior to surgery so that the physician comes in prepared with the right team to go after the disease. Understand that treatment options include both medical and or surgical. And definitely I love seeing and listening to Doctor Payne because the input of our pain psychology is critical as well in the care of our patients. Thank you so much for your attention. I hope that this was helpful.
Margaret Caspler Cianci:
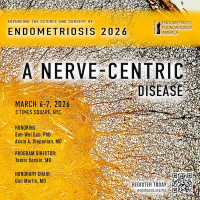
Thank you so very, very much. We really, really appreciate it. And it's one of the topics about re operative endometriosis, particularly that statistics that you showed us that close to 60% after seven years have, after just the hysterectomy, not the Uberectomy, that in fact it comes back. I mean, that is something that we constantly hear from so many people. And so we really appreciate you're giving us those takeaway messages. We do have a number of questions around, again, re operative endometriosis. Let me just say at the onset that from the foundation standpoint, we will be discussing re operative endometriosis at our medical conference, which we had to postpone for March, which is now being rescheduled in November. So we continue to work with the medical profession, also trying to educate them about all of the different elements that you just laid out, because it's so important that there are so many doctors that are not attuned to it.
So we need more surgeons like you and more doctors like you. So thank you for joining us today. One of the questions that we have, and I think it's probably something that we hear quite a bit is from Sonia, who said, "I'm scheduled for my third excision, which was the last one was eight months ago. I'm 38 and now I've been diagnosed with stage four. I only have one ovary left. Will removing this last organ stop my endo? I also take progesterone and that did not slow the growth again. Looking at your first patient who has already had five surgeries, I think we hear this a lot and was wondering if you have any comments to her.
Rosanne Kho:
Right thank you so much for sharing your story with us. So the landmark study that I showed earlier, right? What are the chances of having to undergo another surgery even after both ovaries now have been removed, including the uterus? So that studies show that it's up to 8% when patients were followed over seven year period of time. Let's focus on that the 92% of the time, or the 92% of women who do not end up with another operation at seven years. And we pray that you would be one of those patients, right? So some of the key things to take then would be 1) that you go to someone who's comfortable doing this, with excising, knows what to look for and how to perform the procedure. Hopefully they're able to go in knowing exactly where the disease would be so that complete excision can be done.
So the role of imaging, going in prepared would be key and surrounding yourself with the best support that you can. I go back to the question that was posed to Dr. Payne, in the patient who underwent surgery in addition to current hysterectomy and the type of discomfort now that she has after the bowel procedure is different from the type of pain that she came in with the endometriosis. And I want to emphasize that patients who undergo bowel surgery will take a while before their bowel function goes back to normal. Sometimes it takes three months, others take six months, others take one year, others take two years before they start having the frequency, the urgency and different bowel symptoms that one develops after these surgeries.
Margaret Caspler Cianci:
Thank you, Dr. Kho, it's fascinating. I will say something that Dr. Martin said yesterday, which I completely think is incredibly relevant, and that is that this disease is really difficult to understand, and it is really individual. And I think that we're seeing that whether it's, you know, whether you've had a hysterectomy, not had a hysterectomy, it's just such an individual and difficult to understand disease. So thank you for that. Another question that we've had is from Marguerite. And she wants to know that if she's had her hysterectomy, but keeping her ovaries, an excision by an endo expert. She's scared of the future. She's been pain-free for four years, but it took a very long time for the pain to go away. And so she's worried about the future. And there's also people who are asking, "What are the chances of my getting ovarian cancer?" And some of those questions as well, if you want to address them.
Thank you, Dr. Koh. Interestingly enough, after our break, our next panel, will be talking about the extra pelvic endo. So thank you very much. We know that that is a very, very big topic. So this last question relates a little bit to something we heard yesterday. We had a nutritionist on, and the question comes from Maddie or no, I'm sorry. It was anonymous. But the question is, "I recently had a hysterectomy for my endometriosis. I've heard about changing my diet to suppress any into mitosis that wasn't removed. Is that true? So we were asking you as a surgeon, what you think about diet as well? You know, a nutritionist of course thinks it's very important, but we'd love to hear your opinion on it.
Rosanne Kho:
You know, I have to be very transparent and open here that I am not the nutrition expert. However, there are many, many lines of service now at all the different facets of endometriosis. One that we would have to think of, and I'm strong believer in use of supplements and a good diet in order to maintain our wellbeing. If we think about endometriosis as a chronic inflammatory condition, is there a role in modifying our diets and our supplements to minimize the anti-inflammatory benefits of certain food products? Right? So just to plant that thought, but can I quote you any studies? I can't and I apologize. I would have to go back and listen to our nutritionist expert.
Margaret Caspler Cianci:
Not necessarily, but again, the idea of the anti-inflammatory is so important. So we truly appreciate this again. We will make this available to all of those who've registered so that they can go back and listen again. And if you have additional questions for Dr. Koh, please send them to us@questionsatendofound.org. And we will work with one of our doctors to try to have them all answered in the future. Dr. Koh, thank you very, very much.