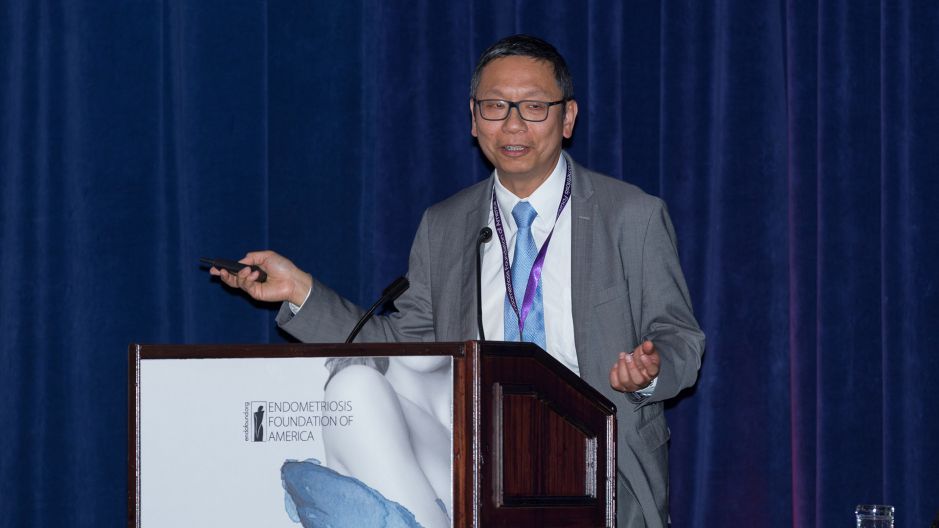
Endofound Medical Conference 2017
"Breast, Ovary and Endometriosis"
October 28, 2017 - Lotte New York Palace Hotel
Cancer Implications for Patients with Endometriosis
le-Ming Shih, MD, PhD
Richard W. TeLinde Distinguished Professor,
Johns Hopkins University
Thank you for the kind introduction. I would like to thank Dr. Seckin's kind invitation for me to have this wonderful opportunity to be here and update you where we are in studying endometriosis. Let me figure out this, so ...
I'm sorry. I'm pathologist, I'm not smart enough.
Okay. Dr. Osler was to say, "He who knows endometriosis knows gynecology." I'm not sure this is true now, but I hope partially this is true. Okay. As we know and we learned from a lot of speakers and literature, that we know that there are at least three different kinds of endometriosis. Okay, the first ... I'm sorry. How can I go back? Okay. I'm sorry. Can we go back?
Okay. I'm sorry. Okay, thank you. All right. We have three kinds of endometriosis. One is endometrioma, here in the ovary. The other one superficial endometriosis, probably coming from the retrograde during menstruation. But the one I'm talking is most of concern is this deep infiltrating endometriosis. It's really a disease of riddle, wrapped in a mystery, and inside an enigma. We know that this [inaudible 00:01:52] endometrioma probably is the retrograde menstruation that sink into the ruptured corpus luteum, and we know that this superficially coating may be directly from the menstrual blood. But how can this deep infiltrating endometriosis, DIE, in this deep of the tissue, of the colon, rectum, urinary bladder et cetera. That's really intriguing.
I'm a pathologist and I am also a cancer researcher, so I hope I can bring different view to this endometriosis field. In cancer research, we study ovarian cancer and [inaudible 00:02:34] diseases. One of the common tools we use is the ... I'm sorry. I hit the wrong one. Okay ... Is we do the whole exome sequencing, or whole genome sequencing, and as you know, there's so many omics that is really a standard of the tool in cancer research. Then we is just thinking, why we just apply cancer research tools to endometriosis and to see what happens.
So, we conduct a study we just publish in NHIN and we analyze total 39 deep infiltrating endometriosis, DIE, and including 24 of them, we do a whole exome sequencing. The rest we do the targeted sequencing, using additional PCR. Okay. We had a total 39 cases here, and we had two cohorts. Cohort-1 is from Johns Hopkins hospital. We do a 24 DIE whole exome sequencing. We can analyze 20,000 genes that coat protein and in great detail, and then we use a normal tissue as a control to rule out any germline mutations. Then we have a Cohort-2 from the David Huntsman group in Vancouver, they have 15 DIE. Then, what they did is, they do the targeted KRAS distal PCR analysis.
So this is all result. We have 39, again, 24 plus 15, and we find that about 80% of this DIE has somatic mutations, and more importantly, about one-quarter of them this DIE totally benign, these genes, they harbor cancer driver mutations, either of KRAS, PIK3CA, and PPP2R1A. As you heard from the previous wonderful talks, that these are cancer driver genes. Basically, mutation means that the mutation only occur in the lesion but not in the normal tissue or lymphocytes, we call somatic mutation. This different from germline mutation, that be a CA1, CA2, or Lynch syndrome et cetera. Okay. Then we have two types of somatic mutations. One is a cancer driver mutations, like these kind of genes or also [inaudible 00:04:59] et cetera, et cetera. There are 125 cancer driver genes in human genomes. If they are mutated in different combination they can drive cancer development, so we call cancer driving mutations. The rest about 20,000 genes, if they get mutated, nothing will happen because they represent the passenger gene mutations. They are just passenger, they are not driver, so they are just bystander, just get mutated for no reasons. We will discuss that.
Okay. This is what we found. So initially, we just do the core of the endometriosis from the paraffin block and we put the needle and take it out. Of course, it is composed of epithelial cells and stromal cells. What we found is ... I'm sorry ... You can see this mutant allele frequency, so if this is heterozygous mutation, you should hit about 50%. You see these 24 cases, most of the mutation number, the allele frequency is very low, so that's means that the mutation is not present in every single cells, in the stromal and epithelial cells, in any given DIE. So, we can confirm the somatic mutation using another technique called [inaudible 00:06:25].
Okay. Then we analyze whether this driver gene is a random event or not. Remember, every single cell in your body, when they divide, they will pick up three somatic mutations, even they are proficient in DNA damage repair. So when you have more cell divisions, you accumulate more and more somatic mutations. Everybody's every cells has a somatic mutation and the number really depends on how many cell division has occurred in the past. Okay. There is one challenge from the cancer driver mutation, but we don't know whether this just hit by chance, or is it has a selective pressure that the DIE try to keep or reserve the cancer driver mutations. We use a mathematical model to calculate that this not random event, meaning the DIE harbor those cancer driver mutation, must force some purpose and we will discuss what is the purpose.
We can skip this one. So basically, you can see that that this is human genes, different genes, and the red one, probably you cannot see here, is the cancer driver genes. If you randomly draw a lottery, 1 out of 100 chances, you will pick out cancer driver genes, but in our case, we have 80 total somatic mutations, but 5 have them has cancer driver mutations. This is highly significant. It's not random, it must have some teleological purpose that they get mutated.
So, when you look back to this cancer driver mutation. KRAS, PIK3CA, ARID1A, and PPP2R1A, they are involved in many cancer pathways. It's just been discussed by outstanding speakers, so I don't need to go over that. But more importantly, I want to show you is this. This is the ovarian cancer map. Okay, we know ovarian cancer is composed of different histological subtypes. High-grade serous carcinoma, low-grade, clear-cell, endometrioid, mucinous carcinomas, and they have a different origins. For example, high-grade serous carcinoma, they are derived from the fallopian tube. Clear-cell endometrial carcinoma, they are developed from the endometriosis. Basically, there is no ovarian cancer in the whole wide world. Ovarian cancer are all imported diseases, either from the fallopian tube to become serous carcinoma, or clear-cell endometrial carcinoma, imported from this endometrium. I want to draw your attention is, those mutations we identified in DIE, they just fit very well to the clear-cell endometrial carcinoma. They are not shared by low-grade or high-grade serous carcinoma, so this has really good support that clear-cell endometrial carcinoma, to some extents, are very related to endometriosis.
Okay. Now we got a somatic mutation. The next most important question we want to address is whether the somatic mutation occur in the epithelial cells or the stromal cells. As remember, the endometriosis is defined by histology as the binary growth pattern which is composed of epithelial glandular component and the stromal cells. So, we do a laser capture microdissection, just take out this epithelial cell only, and we remove the stromal cells for side-to-side comparison. We use the [inaudible 00:10:12] and also digital PCR to confirm this. For example, this case, we find the mutation is only restricted to the epithelial cells. The KRAS, we know we do laser capture, we know there's a KRAS mutation, but not in the stromal. Likewise, in this case, there's ARID1A, which is a chromatin remodeling genes, I will cover that later on, you see the mutation is only restricted to epithelial cell but not in the stroma. That's quite interesting, right? Because people said that endometriosis can coming from the single stem cells where it differentiate into either epithelial cell or stromal cells, but our data did not support the view.
For the microdissect, the DIE in some cases, we find the same thing. The mutations only occur in the epithelial cells. We also using the immunohistochemistry to confirm our findings. This one DIE stromal epithelial cells and this one did not have ARID1A mutations, so as a result, every body are own because they express ARID1A tumor suppressor. But in this DIE, you can see the epithelial cells lose the ARID1A staining. Because of the underlying somatic mutation that make this gene cannot produce any protein products, but stromal cells servicing proton positive control.
We further analyze ... Okay, we have a driver mutation, so you may argue why the driver mutation on occur in the epithelial cells. Well, no brainer, because this KRAS and PIK3CA has also been detected in carcinoma, epithelial-derived tumor, right? So they must confine to the epithelial cells. But currently, we have a new data to show even passenger gene mutation and synonymous mutation, meaning this somatic mutation did not change amino acid, again they're all confined to epithelial cells. Even the passenger and the synonymous mutation only in the epithelial cells, just like driver genes, but not in the stroma.
What does that mean? We can discuss about that. So, there is different hypothesis we can generate from this result. That for the DIE, we think they are circulating endometrial progenitor cells. I don't want to call it stem cell because stem cell, usually we reserve for embryonic stem cells. But we want to use the progenitor cells, that cell can produce the progeny of epithelial cells. We know that menstruation ... why human need menstruation? Because it's a very important tumor suppressor functions. Remember, two weeks after menstruation, the full thickness of endometrium repopulate, right? We see only 10, 12 days, so this must have jillion numbers of cell division. As a result, I just told you, every cell division will accumulate three somatic mutation. The three mutation may hit non-coding area, or the non-important cancer driver gene, then you are fine. But if this three mutation hit any one of the 125 cancer driver, then in the cell get trouble. Okay. So we think that menstruation just get rid of all this accumulated mutated epithelial cells every month. That's why that endometrial cancer is not everywhere. It's important but it's not everywhere.
After the menstruation, the endometrium need to regenerate, need to repopulate. What happen there? Actually, this so fundamental question, right? But actually not many people know exactly what happen there. Our idea is, it's coming from the blood, actually blood progenitor cells from the endometrium. Okay, so this is endometrium here, normal eutopic here. I'm sorry. After menstruation, they will shed the endometrial progenitor cells and some of them will stuck into the blood vessels and circulate in the whole body. So every woman in the reproductive ages probably has many circulating endometrial progenitor cells. Then, after the menstruation, this progenitor cells home in to the endometrium and try to repopulate, so this is very different from the conventional view that, okay, there is a basal layer and there is a stem cell niche where you repopulate, just like colon. We don't think this is very unique from colon regeneration. It's coming from the blood circulating, blood-born progenitor cells.
In terms of endometriosis, endometriosis to me is exaggerated tissue repair problem. Exaggerated tissue repair problem, because if the woman has a menstruation, this progenitor cells, it become more and more accumulated in the body. Somehow they can go astray and stuck in the peritoneal cavity, which they share a similar habitat, so as a result, they think this is normal endometrium but it's not. It's in the colon, it's in the urinary bladder, in the ureter where they develop into endometriosis. That's what our view is about DIE.
Then you are ask one very important questions. Then how about the stroma and epithelial cells? We think ... The epithelial cell, I just told you could be coming form the blood-born endometrial progenitor cells. When the single cells, they stuck into the peritoneal cavity, then they send a signal, we don't know what are those. They recruit bone marrow mesenchymal stem cells to come to the local site, where they become the [inaudible 00:16:25] positive endometrial stromal cells. They are totally from a different roots to map this composite endometriosis. Of course, there is no proof, but I think this is just a hypothesis that we can explain the DIE. Then, the next question is, how about the mutations? Why the stromal cell did not have a mutation but only epithelial cell has a mutations? We know that the mutation is not random, must serve some purposes, so we think, we believe, that the epithelial cells which harbor the cancer driver mutation can give the epithelial progenitor cells better chance to survive ectopically, because it's unlike endometrium, which is their home, right? Now they are in different cities, so the somatic mutation cancer driver can make them better fit into this different environment.
Then, you must experience a lot of patients has multiple endometriosis, so in this 30, we have one patient, we analyze one patient who has five different DIEs. Then we do the laser capture microdissection, do the somatic mutation analysis for KRAS, and guess what? Among this five, we find three of them share the same KRAS mutation. Exactly same mutations in the nucleotide, but the other two we cannot find mutation. May be false negative, whatever, we don't know. That means that either this three DIE share the same KRAS mutation coming from the progenitor cells, very originally, very ancestral [inaudible 00:18:15] from the endometrium. Then they can colonize in the different site into different endometriosis or they coming from one endometriosis KRAS mutation. Then, where they just metastasize, just like cancer, metastasize to the other sites to form another [inaudible 00:18:35] DIE. Actually, we don't know.
Okay. This is our view as a cancer biologist. We think there are expanded clones with cancerous mutation are very common. What happen is, in DIE there is one progenitor cells with KRAS or [inaudible 00:18:56] mutations. Then, they can commit the cells to survive better in a very harsh environment and where they have a very brief clonal expansions. That's why ever epithelial cells harbor the same mutations, but they cannot go too far away because of either telomere shortening, or oncogene induced senescence, or apoptosis, so they stop there. So endometriosis DIE they cannot grow like a tumor, but there is some situations that endometriotic cyst, they forming like 10 centimeter cysts in the ovary, somehow they pick up more mutations. As a result, they have more clonal expansion than the DIEs. But, for the unfortunate patients who has ovarian endometriotic cyst, then they can further accumulate sufficient number of cancer driver gene mutations and for then to become clear cell endometrioid carcinoma. So probably, this is a scenario that happens to a DIE, and this is not the single event alone.
In human body, we have many, many of this mini, minute subchromes with cancer driver mutation but note morphologically, they are normal and phenotypically, they did not [inaudible 00:20:16], but they just exist just like a fossil in your body. You have a lot of mutation in your body, but they will not progress to cancer. That's why the cancer prevention is very important, because you will prevent those clonal expansion and try to block their progression into the cancer.
Okay. So endometriosis, many people say, "Well it could be a cancer because, you see, they have a very highly invasive phenotype. They can metastasize." So to be cancer, or not to be, that is the question. I hope Shakespeare can agree. Okay. To be cancer. If DIE has dissemination, infiltration, invasion, and so called metastasis, and they represent a wound that never healed, right? It's a chronic inflammation, fibrosis, just like cancer. Cancer is a chronic wound, never healed and this is it. We have recidivation, meaning it's always recur. This disease can recur. It's a clonal growth because we found a cancer mutation, so this a very important proof that this is with some cancer phenotype, but we don't want to call endometriosis cancer yet. Then there's a risk for endometriosis-related neoplasms. So this favor that DIE actually has a cancer phenotype, but there is another group that did not favor this is a cancer. Actually, favor it's a benign.
For example, there is not solid growth and it is a controlled proliferation. Cancer is, you cannot control the proliferation, so it become cancer, but for the DIE, they have really low proliferation. It's not fatal. It's non-fatal migration. Normal-appearing morphology. Look under the microscope. If you tell any pathologist this is endometriosis, or endometrium, they cannot tell you if you don't tell them. So morphologically, basically, you cannot distinguish from the pure, normal endometrium. They have very low proliferation, and we do the cancer pathways and they are all negative. So this findings did not suggest that DIE is a cancer.
Okay. You may ask whether those with cancer driver mutation DIE has high proliferation but actually, they are not, so this is very different from cancer research field. We know you have a KRAS mutation, ARID1A mutation, the proliferation will increase, right? Because that's why they get cancer. But in DIE, even they have a cancer driver mutation, they did not proliferate, so they must do something else, right? So this is what we think.
For example, KRAS. KRAS is important in the experimental endometriosis. We know this and that, but the most important thing is, we find in some literature that KRAS mutation may be related to progesterone resistance. Maybe the KRAS mutation is not important to propel cell proliferation into a big mass, but if you treat progesterone, if those patient with KRAS mutation maybe not as responsive.
This another ARID1A which we discovered this gene at Johns Hopkins. It's turn out to be a very important cancer gene in endometrium-related cancer, either as uterine endometrial carcinoma, ovarian endometrioid, or ovarian clear-cell carcinoma. It's very high prevalence, about 50%. It's a chromatin remodeling genes, so in our group, in our laboratory, focus very much on the chromatin remodeling [inaudible 00:24:01] in this gene. When you don't have ARID1A, because of mutation, the chromatin is really close. Very compact. But in normal cell, which has ARID1A, chromatin is more open. So we find that the ARID1A loss and the progesterone expression there is an inverse correlation, and also we do the whole genome [inaudible 00:24:26] in the RNAsik analysis, we find that ARID1A is linked, very closely linked, to the PR signaling pathways.
This data propose that it's very important for us to know what happens for this cancer driver genes do for this DIE. Maybe it's not for their proliferation, but rather for their survival, especially when you have a selective pressure, meaning either hormone therapy, [inaudible 00:24:56] inhibitor, GnIH antagonist and agonist, or progesterone. Maybe that's they play a role over there. I don't want to focus on this because it's been covered previously, so this is all ... Yeah.
But I want to show you one things that's more important, is the summary and the future direction. How can we do endometriosis research given the era of genomic medicine? So basically, I show you that somatic mutation can be detected in most DIE lesions. About one quarter harbor this oncogene or tumor suppressor, which is quite scary, right? Because for the general population, you tell them, "Oh, your DIE has cancer driver mutation." They must be scared, because they think it's a cancer, but it's not. It's more complicated than that. Then endometriosis, we think it is an exaggerated tissue repair as a result of endometrial regeneration. Then this to be tested in the future. Our data suggest the new directions to frame endometriosis research.
For example, question number one. Clinically distinct endometriosis type, like DIE, superficial, and endometrioma, they are similar in their etiology and also their genomic? We don't know, so we are really eager to sequence the endometriotic cyst and also the superficial endometriosis to see whether they have a somatic mutation, number one. Number two, if they have the cancer driver mutations. Question number two. What are the biological role of this driver mutation in DIE? As we just discussed, maybe it's not important for them to become cancer because the cancer incidence in this DIE is extremely, extremely low, but they can do something else and this is we are going to find out, to correlate the genotype and the phenotype, meaning the pain index, the recurrence, the treatment outcome et cetera.
The third question is, can somatic mutation predict clinical outcome response to hormone et cetera? We just discussed, so I think this is require a team effort. It's a collaboration between pathologists, gynecologists, and also scientists to answer this important question. Then, question number four. Can we include molecular genetic findings for new classification of endometriosis? Now endometriosis classification is [inaudible 00:27:40]. It's very confusing and it may not be faithfully refer the biology of endometriosis. Now, we have a better tool. We have a higher resolution. We know what kind of mutation, what gene expression abnormality, also epigenetic abnormality. Maybe in the future we can use a molecular diagnostic to do more precision medicine for endometriosis in women.
Finally, it's whether we can repurposing cancer-like treatment to selected patients with cancer-driver mutation? We know, in cancer, if a KRAS mutation, PIK3CA mutation, ARID1A mutation, we have a cancer drug. We can treat those tumor with those mutation. Like ARID1A mutation, we have [inaudible 00:28:23] inhibitor et cetera. So for those very rare refractory, treatment refractory patient, maybe we can consider to use a low dose of cancer drug to block the specific pathway for their disease. We don't know whether this will be true or not. Finally, whether we can use this knowledge for the potential chemo-prevention of endometriosis. For example, some natural product may block certain pathways of this cancer driver mutation and there is many, many thing that we can think about and we can do together.
Without further introduction, I would like to thank our team. Actually, it's many people, like pathologists, gynecologists, and animal scientists. Do you know who is this person? Gynecologist. Okay. Actually that's the name to be acknowledged in this study and also I appreciate, very grateful, that Dr. Seckin and Endofound can participate in this research and we can come up very nice result to the public.
Thank you very much for your attention.