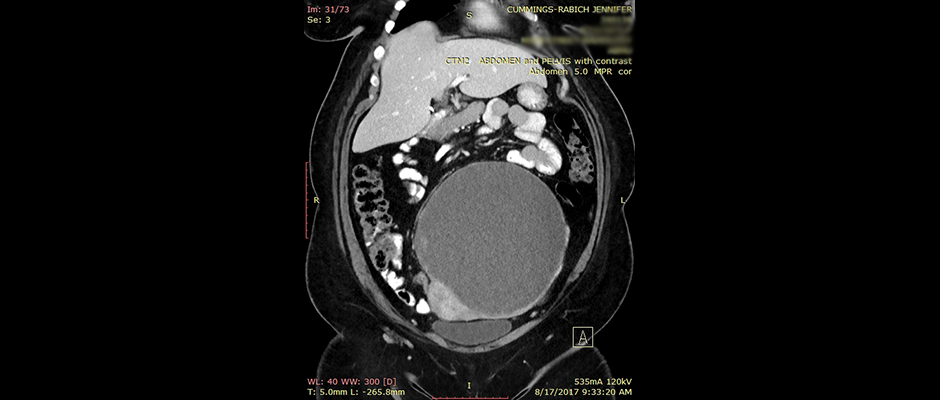
Above, Jennifer Cummings-Rabich shares a CT scan of her pelvis. Inside, her 20-centimeter, basketball-sized ovarian cyst displaced several organs. Pathology later confirmed the mass was clear cell carcinoma, a deadly and rare form of ovarian cancer.
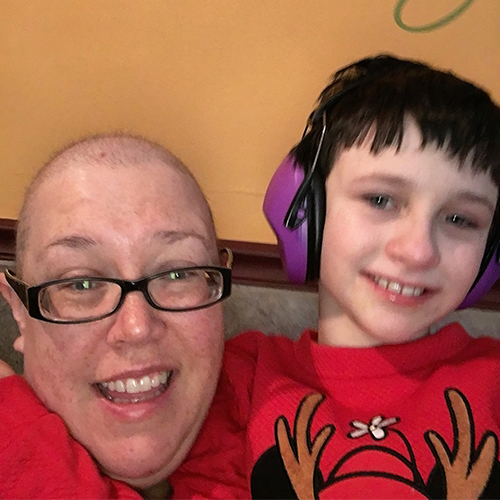
Jennifer Cummings-Rabich of Queens, New York had no idea what was wrong when she started feeling discomfort on the lower left side of her abdomen. She couldn't lay on her stomach. A stay-at-home mom to her daughter Shaylie, 9, who has autism and ADHD, Cummings-Rabich put her pain aside, telling herself, "I'll deal with it later.”
That was February 2017, but by July, the pain was so severe that she could barely walk. Her OB-GYN asked her if she was pregnant. After an examination, Cummings-Rabich learned she was carrying around a 20-centimeter mass, roughly the size of a basketball, on her left side.
“I just stood there and [my OB-GYN] goes, ‘Jennifer, you’re very calm.' And I said, ‘I need to pay extra attention to what you’re telling me, so I can relay this to my mother and husband. So, I can’t afford to fall apart right now. I’ll fall apart later,’” Cummings-Rabich, 45, tells The Blossom.
She then took her mother along to a gynecological oncologist at New York Presbyterian Hospital of Queens to get a sonogram. What they saw shocked everyone in the room—the mass took up the entire screen. “My mother worked for an OB-GYN for at least 20 years, and she almost fell off her chair when she saw this thing,” she adds.

By September, Cummings-Rabich was on the operating table at Memorial Sloan Kettering Cancer Center. She was in surgery for nine hours; it took surgeons five hours just to remove the mass.
Pathology revealed the tumor was a rare form of ovarian cancer: stage 1C of ovarian clear cell carcinoma.
The deadly clear cell lives up to its name. When viewed under a microscope, the cancer cells look clear.
“The surgeon told me, about five percent of their patients with clear cell had endometriosis,” she says.
Following the removal of the tumor, doctors performed a total hysterectomy and bilateral salpingo-oophorectomy, or the removal of not only the uterus but both ovaries to minimize the chance of cancer's recurrence.

In November, Cummings-Rabich began six rounds of chemotherapy lasting three months. And her journey to remain in remission is far from over. Every three months for the next two years, she'll need to see her oncologist for bloodwork, and CT scans.
A history of pain
Cummings-Rabich suspects she had undiagnosed endometriosis during her teenage years.
“There were times that I would have my period and I would have a cold sweat; I would turn as white as a sheet,” she recalls. “I would just be rolling around in pain.”
It took longer than a decade to learn what was going on inside. At the age of 34, during a March 2008 laparoscopy, her doctor found an endometrioma inside her left ovary, and adhesions that bound her bowels. Post-op, she started injectable fertility treatments, and Intrauterine Insemination (IUI), eventually getting pregnant with Shaylie. Soon after the birth, she says her periods weren’t as heavy, but the pain was “still incredible.” By 2016, she experienced rectal bleeding and suggested a hysterectomy, something that her doctor at the time said would cause too many problems.
While it was clear to Cummings-Rabich that her endometriosis symptoms were worsening, ovarian cancer never crossed her mind. According to the American Cancer Society, a first-degree relative with ovarian cancer increases risk four-fold, but ovarian cancer of any kind was nowhere to be found within her family history. There were, however, other malignancies. She had an uncle who had leukemia; an aunt who had pancreatic cancer; her father had prostate cancer; another aunt had lymphoma; her grandfather had prostate cancer and head-neck cancer; an aunt had Stage 3 colorectal cancer; a cousin had endometriosis.
Endometriosis and the risk of clear cell carcinoma
Each year, about 20,000 women in the United States develop ovarian cancer, and it causes more deaths than any other cancer of the female reproductive system, according to the Centers for Disease Control and Prevention. In 2018 there will be an estimated 14,070 ovarian cancer deaths in the US alone, according to the American Cancer Society.
But a link between endometriosis and clear cell is hazy at best. A 2016 report in Menopause Review studied 394 patients in Poland who had received ovarian cancer operations. Researchers found clear cell carcinoma in only 0.02 percent of the patients, but they couldn’t draw a direct cause-and-effect relationship between endometriosis and cancer.
Dr. le-Ming Shih, MD, Ph.D., the Richard W. TeLinde Distinguished Professor in the Department of Gynecology and Obstetrics at Johns Hopkins University, tells The Blossom that the “chance to develop an ovarian cancer from endometriosis is slim.” Shih says he has been studying endometriosis and endo-related cancers for 18 years.
He adds that if a woman has a big ovarian endometriotic cyst, she should see a gynecologic disease specialist to figure out the risk of ovarian cancer. "Unfortunately there are few symptoms or signs at an early stage, so ovarian cancer is called the 'silent killer.' But if endometriosis patients have abdominal bloating or fullness, changes in bladder or bowel habits or abnormal uterine bleeding, they should consult with their gynecologists." Shih adds that abdominal sonography and a CA125 blood test, which measures the cancer antigen in one's blood, can also determine a patient's risk for ovarian cancer.
Still, he says more work needs to be done to understand the link between endo and clear cell. Right now, scientists are looking at how endometriosis could lead to cancer at the molecular level.
“Once we have a better idea from the molecular genetic studies, we will then be at a better position to develop a test for early detection of endometriosis-associated ovarian cancer, leading to a cure before the cancer arises."
Rebirth in remission
Although Cummings-Rabich says she sees a therapist and currently is on Zoloft to deal with the stress that has come from her health issues, she says she has "never felt better" now that her basketball-sized mass, and her uterus, are now gone. She's also sporting a brand-new look thanks to her hair growing back after chemo.

“This past almost year of not worrying about periods or anything like that—it’s been a weight lifted,” she says. “Physically, without having to deal with that every month, I feel great.” But the best feel-good news of all? Doctors have told her her prognosis is good.
Now, Cummings-Rabich says she wants other endo women to learn from her mistake of shrugging off the warning signs her body showed her.
“If you’re a mom, we tend to put ourselves last on the totem pole,” Cummings-Rabich adds. “Anybody that I know that has endometriosis, I'm telling them to stay on top of their health, to stay on top of their doctors, because you don't want this. You definitely do not want this."









