
After news spread of Lena Dunham’s total hysterectomy to treat her endometriosis, a global conversation began to unfold: Is a hysterectomy an effective form of endometriosis treatment?
“There is no certainty that a hysterectomy will rid a patient of their endometriosis,” Harry Reich, informally known as “the father of endometriosis,” tells The Blossom. Reich is also credited with performing the nation’s first laparoscopic hysterectomy for endometriosis in 1988. “It is in the case of diffuse adenomyosis, or endometriosis throughout the wall of the uterus itself when a patient starts to consider a hysterectomy as an option to relieve the pain associated with this form of the disease.” Reich, who served as the previous director of advanced laparoscopic surgery at Columbia Presbyterian Medical Center, also emphasizes that it is imperative doctors remove endometriosis in areas outside of the uterus at the time of performing the hysterectomy.
Dr. G, an OB-GYN who specializes in the surgical treatment of endometriosis, agrees.
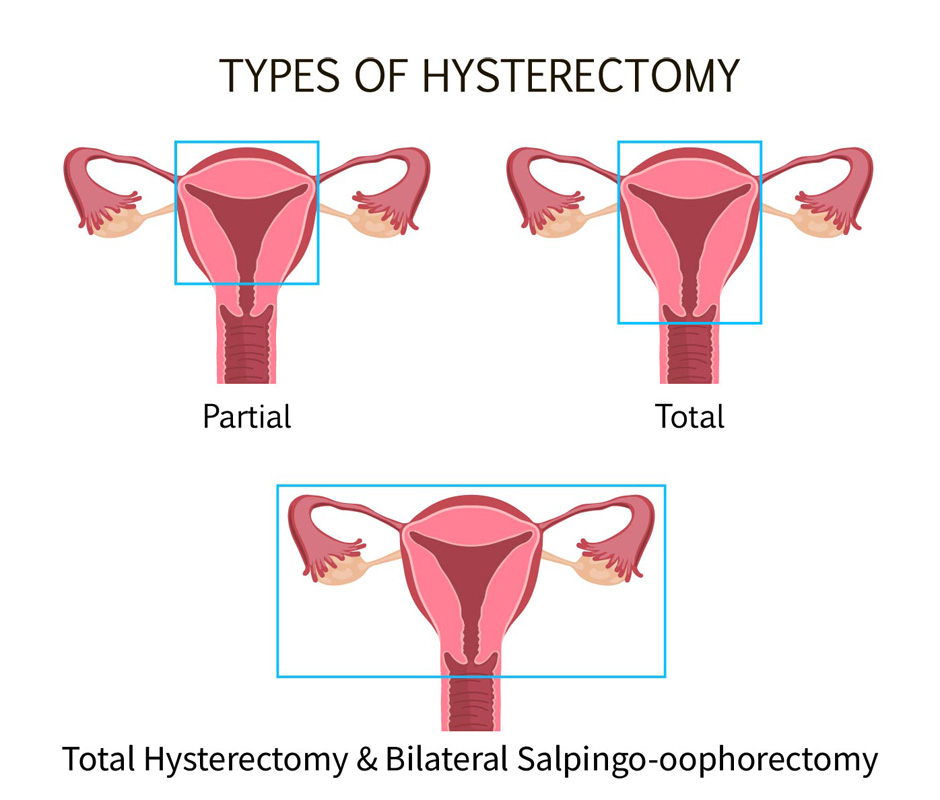
Partial hysterectomy: Removes the uterus, not including the cervix. A patient may choose to undergo this form of hysterectomy to preserve a healthy cervix.
Total hysterectomy: (Lena’s choice) Removes the uterus, including the cervix. A patient may choose to undergo this form of surgery if there is endometriosis involving the cervix and they also wish to preserve the ovaries for possible IVF treatments and future surrogacy.
Total hysterectomy & Bilateral Salpingo-oophorectomy: Removes the entire uterus, fallopian tubes, and uterus. A patient may choose to undergo this form of surgery if they do not wish to become pregnant in the future and want to limit their risk of ovarian cancer.
“Oftentimes, doctors may fail to recognize the disease that lies outside the scope of the hysterectomy procedure, or outside of the uterus,” G tells The Blossom. “It is essential, even in the case of a hysterectomy, that excision of endometriosis is always performed at the same time in order to treat the rest of the disease within the pelvis. If a surgeon performs a hysterectomy, but still leaves lesions behind elsewhere, patients are at risk of having persistent symptoms.”
Dan Martin, a retired OB-GYN and professor emeritus at University of Tennessee Health Science Center says he has 44 years of experience in operating on endometriosis patients. “The first thing you want to do is to try and avoid a hysterectomy,” says Martin. But in Lena’s case, “for someone who has had multiple surgeries that didn’t work, hysterectomy is an option.” Many studies abound, adds Martin, claiming that hysterectomy “for chronic pain works between 50 percent to 95 percent of the time.”
Lena’s story and the debate surrounding hysterectomies serves as a springboard to a much larger conversation that patients and physicians can begin to have as they work together to find an effective form of treatment for a disease that has been an ongoing struggle for so many women worldwide.
While Lena underwent a total hysterectomy, there are also partial hysterectomies that do not remove the cervix and hysterectomies that remove the ovaries and fallopian tubes (also known as, a bilateral salpingo-oophorectomy). “What form of hysterectomy a patient chooses to undergo is a decision made by the patient, but also must be discussed with one’s physician depending on if endometriosis is involved in these specific areas,” says Dr.G.








