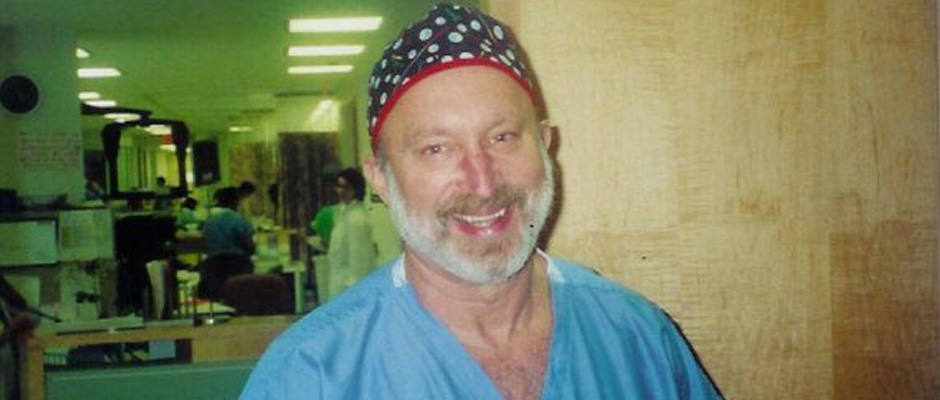
Introducing our brand-new advice columnist Dr. Harry Reich. If the name sounds familiar, it should; he’s EndoFound’s Honorary Medical Director Emeritus and Senior Medical Advisor. During his 30-year career as an OB-GYN specializing in endometriosis, Dr. Reich has performed 4,000 gynecologic laparoscopy procedures and taught scores of endometriosis specialists how to properly excise the disease, earning him the informal title “the father of endometriosis.” Do you have a burning question for Harry? E-mail him at harry@endofound.org or visit EndoFound’s official Instagram, Facebook or Twitter, tag us and ask a question with the hashtag #askharry, and you could see your answer featured here!
@Cindy L., via Facebook, asks: I would like to hear about women who are post-menopausal, post-total hysterectomy (no ovaries or uterus), who still have endo pain. How can I get help? I have seen two endo specialists, and neither want to do surgery. What else is there? I would never do Lupron again, or any medicine like it. I live on Percocet and muscle relaxers, which I hate. What other options do I have? I do not want to live the rest of my life like this! I am 59 years old.
Most surgeons operating on deep cul-de-sac endometriosis leave much of the disease behind on the rectum and the top of the vagina where it was joined to the cervix. Beware of the surgeon who uses the term "intrafascial hysterectomy" as this technique leaves behind any rectal disease. This is especially common if a cup was used at the junction of cervix and vagina to separate them during laparoscopic hysterectomy.
Here are some helpful points to remember.
- Post-menopausal women still make estrogen from peripheral fat and, in fact, remaining endometriosis makes its own estrogen. This estrogen drives a chronic inflammatory response from the endometriosis at the top of the vagina and anterior rectum, and the result is persistent pain.
- Referring back to my last correspondence, a rectovaginal examination will often disclose the diagnosis in cases like yours. To reemphasize what I said before, a rectovaginal examination gives the examiner the ability to check the area between the top of the vagina and the rectum and feel the uterosacral ligaments, if they are attached to the top of the vagina, as they should be after hysterectomy. It also gives the examiner a chance to find out where the patient hurts.
- The treatment that I recommend is to excise the scar tissue at the top of the vagina. The technique that I have described relies on inserting a probe into the vagina so that one can see the thickened old scar tissue through the laparoscope. This scar, often left behind from hysterectomy, is usually closed horizontally by most OB-GYN's. (I've always closed the vagina vertically). I excise the scar tissue and repair the hole, or defect, in a vertical fashion attaching the uterosacral ligaments to the vagina, across the midline, to elevate it. This gives the vagina more support, reducing prolapse and uncomfortable contact with the deepest point of the vagina during sexual activity. In my experience, this technique almost always works.
- If the rectum is involved, various procedures including local excision, anterior discoid resection (which I invented), and bowel resection are available and may be considered.
- Never use Lupron again—or ever!
Editor’s note: The opinions, beliefs, and viewpoints expressed by Dr. Harry Reich in this column are solely his own and based on his experience.









