What happens when a perfectly healthy woman suffers multiple episodes of pneumothorax, or, lung collapse? A medical mystery quickly unravels and leading endometriosis excision specialist and EndoFound Co-Founder Dr. Tamer Seckin is called in to help unveil the surprising true cause: endometriosis.
The Woman Was Fit and Healthy, Why Did Her Lung Mysteriously Collapse?
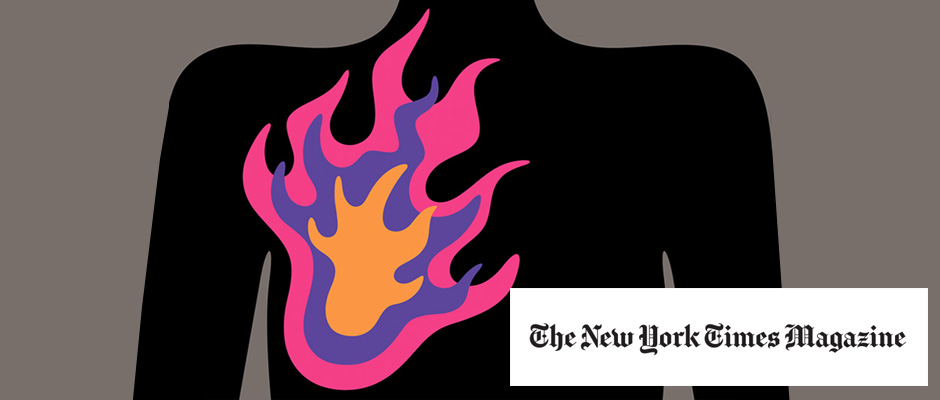
credit: Illustration by Andreas Samuelsson
“Are you O.K.?” the man asked his wife. It was 2 a.m., and he’d awakened to find the bed next to him empty. He found his 45-year-old spouse in the living room of their weekend house up the Hudson River from New York City. She had an oxygen meter on her finger and a worried look on her face. “I can’t breathe,” she told him. She’d had chest pain and felt short of breath in the past, but her oxygen had never been this low — down to 89 or 90 percent. And the right side of her chest felt as if it were on fire.
She wanted to tough it out until morning so that they and their two young daughters could drive back to Manhattan where her doctors were — the ones who had been treating her since her right lung collapsed and all the trouble began two years earlier. That first time had been nothing like this. Back then, there was a strange click, then a feeling that something had moved. It wasn’t painful, just odd. A few days after that, she developed a cough. Her doctor thought she had a virus. When she got worse, he prescribed an inhaler. A few more days passed, and she felt out of breath just walking to the bathroom — odd for a woman who usually exercised daily. Her doctor ordered a chest X-ray and saw to his surprise that her right lung had collapsed.
Deflated Lung
She had, he explained, a pneumothorax — literally, air in the chest. It happens when there’s a tiny rupture in the lung. The air rushes out into the surrounding space, and the empty lung collapses. She was admitted to Lenox Hill Hospital the next day. A tiny catheter was inserted between her ribs into the space around the lung. The air was sucked out, allowing her lung to re-expand.
But why had she gotten this leak in the first place? She didn’t smoke, which is the most common risk factor for developing a pneumothorax. None of the tests indicated any type of lung disease, another significant risk factor. And though there are a number of inherited diseases that can predispose a person to developing a pneumothorax, no one in her family had any of them. After four days and no answers, her doctor concluded that she’d had a spontaneous pneumothorax. These are rare but are more likely to be seen in tall, thin, athletic individuals — like her — and don’t usually happen more than once.
Another Odd Chest Feeling
But a year and a half later, while at work, she felt that same immediately recognizable click and shift in her chest. An X-ray revealed another pneumothorax. At Lenox Hill Hospital, her lung was again re-expanded, and Dr. Byron Patton, a thoracic surgeon, recommended a procedure known as pleurodesis, in which the lung is mechanically attached to the surrounding sack called the pleura, so that even if the lung developed another leak, it wouldn’t collapse.
Over the next half-year, the patient continued to have episodes of chest pain on her right side. Each time she had a twinge or stab, fearing another pneumothorax, she would call her doctor, and he would send her to the E.R. for an X-ray. It happened almost 20 times. The X-rays, though not exactly normal, did not show evidence of new leaks — until one day in May, when a chest X-ray showed yet another, albeit small, pneumothorax.
Why was this happening? The patient asked Patton whether the lung problems could be related to the hormone therapy she’d had for in vitro fertilization (I.V.F.). It was really the only new thing in her life before all this started. It had taken nine fertilizations and nearly three years, but she finally became pregnant four years earlier and now had twin girls. Patton didn’t know of any link between pneumothorax and I.V.F., but there was a link, albeit rare, between pneumothorax and endometriosis — a disorder in which tiny dots of the inner lining of the uterus tissue, known as endometrium, move into other parts of the body. Women who have endometriosis can have episodes of pneumothorax if those cells make their way past the diaphragm into the chest.
This endometrial tissue, like that in the uterus, changes with the monthly cycle of estrogen and progesterone, causing pain and sometimes bleeding. In the chest cavity, it could cause what was called a catamenial (derived from the Greek for monthly) pneumothorax. But did her episodes of pneumothorax come with her period? She wasn’t sure.
Targeting Hormones
Patton had suggested starting birth-control pills to suppress the hormonal changes. She began taking them three weeks before the horrible night at her weekend home, which left her with difficulty breathing. First thing the next morning, her husband carried their sleepy children to the car. She carried the oxygen tank she got earlier that spring — just in case — and they set off for the drive to Lenox Hill Hospital. They stopped to pick up her mother on the way.
At the hospital, an X-ray showed that her right lung, which just weeks before had a small pneumothorax, had now completely collapsed. Patton was shocked. The pleurodesis hadn’t worked. The patient had been reading about catamenial pneumothorax, and even though hormone suppression hadn’t been effective, she still thought this was what she had. Her mother found a gynecologic surgeon at Lenox Hill, Dr. Tamer Seckin, who specialized in the diagnosis and treatment of endometriosis. Mother and patient urged the two subspecialists to work together in the operating room, and they agreed.
In the Operating Room
The operation, which involved both doctors, took five hours. Seckin went first. He looked in the abdomen and pelvis and found many endometrial implants. He saw small patches of wayward cells on the bladder and the intestines and scattered across the abdominal and pelvic walls. But he did not see any on the bottom side of the diaphragm, the muscle that separates the abdomen from the chest. Although there was evidence that she had extensive endometriosis, it wasn’t clear if it was the cause of her lung collapse.
Then it was Patton’s turn. He would examine the chest and lungs. The patient was placed on her left side, and the camera and surgical instruments were inserted between her ribs into the right side of her chest. Patton carefully examined the smooth, curved upper surface of the diaphragm. Directly below the lung there was a patch of purple tissue, a little smaller than a dime. Were those the endometrial cells? Patton cut out the abnormal-looking tissue then sewed up the hole. He scanned the lung, from top to bottom, and found another small patch of abnormal-appearing tissue, which he cut out as well. The samples were sent to the pathology lab. He then fastened her lung to the pleural surface of her chest again. Before the operation was finished, the results were back from the lab. The tissue on the diaphragm was endometriosis. She had catamenial pneumothorax disease.
Recovery was slow after the operation, but the patient felt less anxious because she knew the cause of her lung problems. In a second operation, Seckin was able to remove all the visible endometrial implants. Still, there was no way to guarantee that she wouldn’t develop more unless the source of the implants, her uterus, was removed, along with her ovaries. It was a tough decision. But since she wasn’t planning to have more children, she felt it made sense.
That final operation was six months ago. And the patient says her life is slowly coming back. She jokes that after all these chest and abdominal operations, she looks as if she were in some kind of knife fight. And though her chest still feels tight, it’s good to be able to breathe.
Editor's note: This story originally appeared on nytimes.com