What is gastrointestinal distress due to endometriosis?
The fourth fundamental symptom of endometriosis is irregular bowel movements, mainly highly painful ones. A bowel movement is when your stool passes through and out of your body after the food you have eaten has gone through your digestive tract. Gastrointestinal distress is not limited to painful bowel movements, but can include the following:
-
Constipation
-
Diarrhea
-
Nausea and Vomiting
-
Bloating and Gassiness
-
Rectal bleeding or blood-streaked feces
How do painful bowel movements differ from endometriosis?
What needs to be understood about this symptom is the severe level of pain that can come with it. Patients with endometriosis experiencing irregular bowel movements often describe their pain as sharp, like “cuts with razor blades.” Painful bowel movements, along with symptoms of constipation during menstruation or pain during sex, are significant signs that endometriosis is located in the large bowel. Endometriosis symptoms are unique in that they often coincide with one’s period. If a patient experiences painful bowel movements uniquely during menstruation, this is something to mention to their doctor.
How does endometriosis cause gastrointestinal distress?
How endometriosis causes gastrointestinal distress is not exactly clear, however, there is little doubt that it can be found in the bowels and bladder. These lesions, whether putting pressure on the outside of the intestines or stiffening the rectum, can cause a great deal of pain, especially during the menstrual period. Common areas where endometriosis can infiltrate and cause gastrointestinal distress include:
-
Peritoneum: One of the most common sites for endometriosis to be found, this lining of the intestines can give all the same symptoms of bowel endometriosis cases.
-
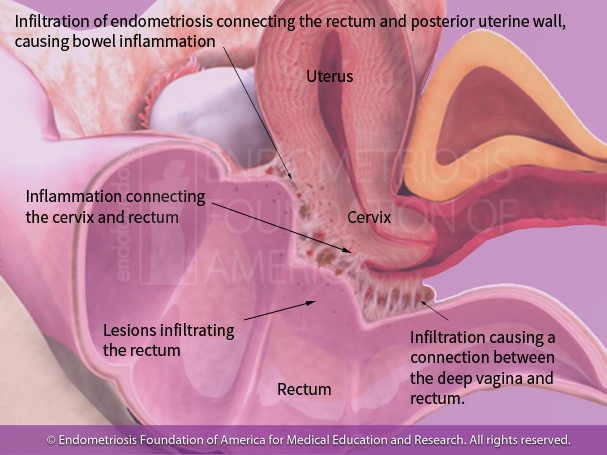
Clinical interpretation: -Lesions to the posterior cul-de-sac, infiltrating and connecting both the posterior uterine wall and rectum. This causes rectal and bowel inflammation and pulls the rectum up towards the vaginal wall and mid portion of the uterus.
Symptoms this will cause:
-Constipation
-Painful bowel movementsCul-de-sac (pouch of Douglas): This area lies between the posterior uterine wall and the rectum. It is a common site for endometriosis to manifest itself and can often cause painful bowel movements and constipation, due to the pressure these lesions apply to the rectum. Patients can also experience painful sex as this area is near the posterior vaginal canal.
-
Rectum: Endometriosis implanting the rectal wall often cause severe painful bowel movements, constipation, and even rectal bleeding. Lesions can also lay in the perianal area (directly behind the anus), which can often cause back pain.
-
Colon and small intestine: Endometriosis can latch onto the outside of the intestines, both large (colon) and small. It is important to note that these lesions cannot be spotted by a colonoscopy as they are on the outside of the bowel walls. Rather, bowel intestinal endometriosis requires a skilled surgeon with a keen eye to what is commonly referred to as “running through” the intestines and checking for lesions.
-
Appendix: The appendix is a common organ for endometriosis lesions to spread. Their symptoms often present in the form of gassiness, bloating, and pain, particularly in the right lower quadrant. Due to its susceptibility to endometriosis and the highly held notion that the appendix is likely a vestigial structure (lacks many functions and specific use due to evolution), it is not uncommon for surgeons to perform an appendectomy (cutting out the appendix) during laparoscopic excision surgeries.
Endometriosis can only exist in the reproductive system (i.e. fallopian tubes, ovaries, and outer uterus.)
Endometriosis is strictly defined as endometrial-like tissue found outside the uterus. While it typically resides in the reproductive system, it can also spread to the bowels, bladder, and most commonly the peritoneum (lining of the abdominal cavity)
Why is gastrointestinal distress often misdiagnosed in endometriosis patients?
Many endometriosis patients who report gastrointestinal symptoms are often misdiagnosed with diseases such as inflammatory bowel syndrome (IBS), Crohn’s disease, and appendicitis. This is because endometriosis that spreads to the intestines will often present many of the same symptoms as the other diseases, such as painful bowel movements, constipation, nausea, and vomiting. A misdiagnosis is not so much a matter of good versus bad provider, but rather a physician’s lack of proper training to rule out diseases such as endometriosis. If a woman is experiencing her gastrointestinal symptoms simultaneously with her menstrual cycle, it could be a key sign indicating endometriosis. Nevertheless, doctors are not taught to ask such questions and in turn, patients may go years without receiving a proper diagnosis. This is why it is crucial for further awareness of endometriosis in both the common public and the medical community.
Constipation, nausea and vomiting, and other bowel issues are strictly due to IBS and other gastrointestinal diseases.
Endometriosis patients can often be misdiagnosed as having IBS, Crohn's Disease, or appendicitis when their GI symptoms are really due to endometriosis.
How to manage gastrointestinal symptoms caused by endometriosis?
Some patients have found that the pain due to gastrointestinal distress is manageable. Through adopting certain lifestyle changes and seeking proper professional help, many patients have been able to find relief in some of their symptoms, namely gastrointestinal distress. Such treatment options include:
Holistic approach: Patients have reported improvements in their symptoms through diet change, namely avoiding red meats, processed foods, and heavy dairy-based products, along with regular exercise. There are many proposed diets for endometriosis patients and it is important to remember when experimenting with holistic approaches, there is no one right answer but rather every patient is different. It is important for a patient to decide on the diet and exercise regime that is best for them, keeping in mind that these measures are for symptom relief, and do not replace well-performed surgery. Nevertheless, when coupled with thorough excision surgery, patients have found holistic approaches highly helpful in their management of GI endometriosis symptoms.
Surgical approach: Laparoscopic excision is the most definitive form of endometriosis surgery. Nevertheless, in endometriosis patients who are experiencing gastrointestinal distress, it is important to note the need for an experienced surgeon. Endometriosis that infiltrates the bowels, rectum, and other organs is not easily removed. It requires a surgical team approach with not just the expertise of a gynecologist, but also that of a gastroenterologist. The surgeon(s) must be comfortable running through the intestines, examining the cul-de-sac and rectum fully, and above all else be cable of reconstructive surgery for areas that have been operated on.
The care needed to discuss GI symptoms
It is never easy for someone to talk about something as personal as her bowels. This is why despite knowing something is wrong, many patients will attribute it to their period or as simply normal. Even when an individual has the tells their doctor about this very personal symptom, they may be rebuffed and told that it is no big deal or is due to a misdiagnosis such as IBS. Doctors can easily recognize endometriosis that involves the appendix, but experienced gynecologic surgeons, as well as general surgeons, often miss endometriosis of the intestines, such as the rectum and sigmoid. Even gastroenterologists almost always miss endometriosis located in the bowel during a colonoscopy. This is why women experiencing severe pain, especially during menstruation and along with constipation, should speak to their doctor. In the case that the doctor is not responsive to these symptoms, patients should make it a priority to find another provider.
References
-
Malin Ek et al., "Gastrointestinal symptoms among endometriosis patients- A case-cohort study." Bio Med Central Women’s Health. August 13th, 2015
-
Nasser S Al Oulaqi et al., "Endometriosis of the Appendix." African Health Sciences. September 8th, 2008.
-
CE Lee et al., "Factors Associated with Severity of Irritable Bowel Syndrome Symptoms in Patients with Endometriosis." National Institute of Health, PubMed.gov. September 1st, 2017
-
Are there contributing factors to the co-presence of Irritable Bowel Syndrome and Endometriosis?, EndoNews.com
- Bowel Endometriosis & IBS, drseckin.com