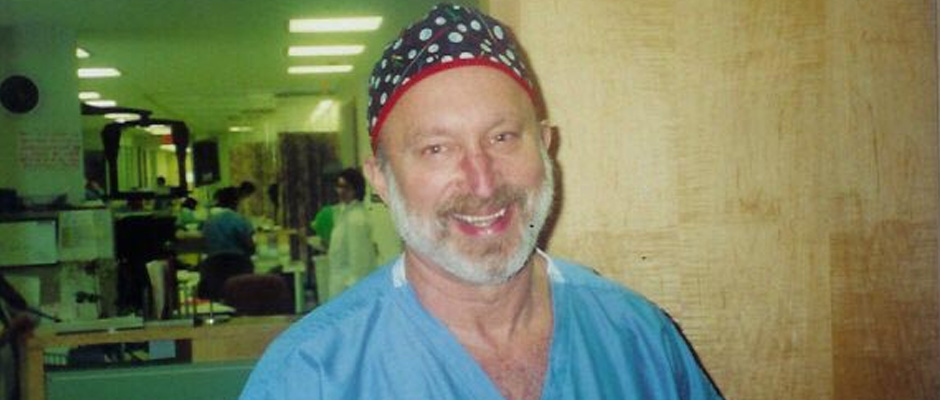
Do you have a burning question for EndoFound’s Honorary Medical Director Emeritus and Senior Medical Advisor, Dr.Harry Reich? E-mail him at harry@endofound.org or visit EndoFound’s official Instagram, Facebook or Twitter, tag us and ask a question with the hashtag #askharry, and you could see your answer featured here!
I've spent decades surgically excising endometriosis from thousands of patients. My extensive experience in the OR has led me to firmly believe that the disease is present from birth, unlike Sampson's Theory of Retrograde Menstruation, which suggests that menstrual blood refluxes, or reverses, back through the fallopian tubes and into the pelvic cavity.
So here it goes. My Harry's Theory of Endometriosis, if you will.
Some cells that are destined to get into the inside of the uterus don’t make it that far. They get close. Like on the rectum, the back of the vagina, and the surrounding ligaments and structures. Throughout your lifetime, these endometriosis-like cells cause a chronic inflammatory response every month resulting in the deposit of fibrotic scar tissue around the endometriosis glands.
Here's the lifespan of endo:
Birth to 10 years: Endometriosis cells lay dormant as they are dependent on ovarian hormones.
Age 10 to 20 years: The inflammatory process from the endometriosis cells begins when the ovaries start to work, causing menstruation. For the surgeon, it is almost impossible to identify the endometriosis cell areas because of the lack of surrounding scar tissue. The areas are too small to see. They are microscopic at this stage. Because of the problems in identifying the endometriosis lesions at this stage, the best approach may be oral contraceptives for painful periods, not surgical intervention.
Age 20 to 30 years: By now, some fibrous, scar tissue has resulted from the chronic, continuous inflammatory reaction that started with periods, making identification much easier. Pre-op, the surgeon can detect them with a rectovaginal examination where one finger is inserted into the vagina and another into the rectum. If the patient complains of tenderness in an area, it's time to zero in on it. The surgeon can now excise the specific endo lesions that have declared themselves. These lesions are tiny.
Age 30 and up: Lesions are now much larger, often the size of a marble, and causing the patient much tenderness. The doctor can sometimes feel them while performing a rectovaginal examination. The scar tissue surrounding the endometriosis gland is the key for successful excision of the disease. The surgeon needs to remove the endo at the junction of scar tissue and normal tissue. If done correctly, excision often cures endometriosis. Yes, you read that right! I believe that proper and thorough excision surgery, as I have done for decades, cures endometriosis. And the pain relief is immediate.
Please note that many OB-GYN's have not seen the full gamut of development of this condition. They see mild cases for painful periods or infertility in young women.
RELATED: Ask Harry: Endometriosis Is Overdiagnosed
@the.vegan.jew asks: Do you think it’s wise to get a six-month follow-up ultrasound after laparoscopic surgery to see if anything has grown back? Also, have you heard of any diet/supplements to be particularly helpful for managing endometriosis? For example, I’ve heard removing dairy helps (which I already do), and DIM helps with overproduction of estrogen.
I see no reason for getting an ultrasound six months after laparoscopic endometriosis surgery. The major determination on what to do revolves around your symptoms. If there is no pain, consider seeing your GYN in one year. If you are having pain, I would suggest a rectovaginal examination to determine the area of pain and whether another operation is needed. An ultrasound determines only whether there is a cyst in the ovary and most ovarian cysts are from normal ovulation. To answer your second question: I do not believe there is any dietary supplement that is helpful in managing endometriosis. I know of no dietary supplement that either promotes or reduces endometrial glands.
RELATED: Ask Harry: Help! I Have Endometriosis Pain After Surgical Menopause
@christinachachaday asks: How common is it to have endometriosis come back after successful excision and total hysterectomy with ovary removal?
Many surgeons do a hysterectomy with ovarian removal without removing the endometriosis. If endometriosis remains, it may cause symptoms. So the answer to your question revolves around how much endometriosis the surgeon removed, and does any remain? Ask your surgeon for a copy of the pathology report to see how much endometriosis was actually removed besides the uterus and ovaries.
@mailoyinda asks: Does the chocolate discharge in someone with endometriosis have any health implications?
A chocolate discharge has no relation to endometriosis. It is related to the length of time that blood remains in the uterus after shedding of its lining during the menstrual period.
Editor’s note: The opinions, beliefs, and viewpoints expressed by Dr. Harry Reich in this column are solely his own and based on his experience.









