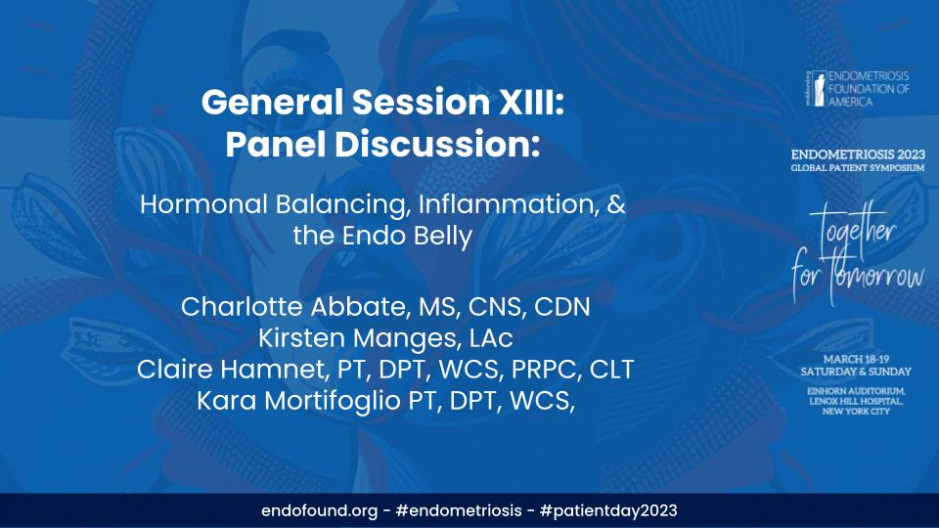
Endometriosis 2023:
Global Patient Symposium
Together for Tomorrow
March 18-19, 2023 - Einhorn Auditorium, Lenox Hill Hospital, NYC
Thank you all. Um, okay. So I wanna start with Endo Belly. Okay. Because that is a, it's a hashtag, it's got a lot of, if you just look it up online, there's a lot to it. But I've experienced it, you can look three months pregnant, you're not, you could try everything, drink water for a day and still have this endo belly. What is it? What is endo belly? Can anyone take that <laugh>? So
A lot of times you're witnessing the inflammation, so you're seeing that accumulation of fluid and you're seeing that accumulation of inflammation, of that tissue swelling. The best thing we can do is really help relax our bodies, take time to ourselves, but food-wise, you know, your triggers, you know the foods that bother you the most and try and stay away from those. Um, but also maintain diversity in your diet. You know, keep up a regular food like intake, like have three meals, have your snacks. But definitely try and avoid those trigger foods for sure. And hydration, I know it doesn't make it go away, but hydration definitely helps. And actually a really cool thing that we're seeing in some recent research is the benefits of different colored foods for endo belly. Um, not specifically endo belly, but specifically inflammation. So I like to look at them together. And eating different colored foods gives you different phytonutrients. And what those colors and phytonutrients do is they help to quench that inflammation and they also help to feed the beneficial bacteria in your gut, which are really supportive in lowering that, uh, that bloat. So
That's, that's great on a nutritional level. And then in terms of, of pt, is there anything that can be done to help manage, um, some of that inflammation going on?
Yeah, definitely. So, um, at pelvic floor physical therapy we can help you work on visceral mobilization, which is getting the organs to move. So your bowel, your small intestines, um, because those can get kind of stuck together when you have inflammation or pain from endometriosis. Um, and then the other piece of it is that with all of the pain and the inflammation, your pelvic floor muscles can calm very tight. Um, and so it doesn't allow you to empty your bowels completely. So, um, if we can allow you to relax your muscles, you'll have some full bowel movements as well as be able to pass gas, which will help decrease the pressure and the swelling in your belly.
Um, also I like to look a lot at different kinds of lymphatic techniques that can be done to kind of help move along inflammation or whatever may be part of end Nobel, um, in order to kind of keep things moving, like that's definitely not a long term, long term fix as much as what everybody else has already set up here. Um, but it's certainly something that can help improve quality of life while working on these other things. So, mm-hmm.
<affirmative> and what plays a large role in the hormonal imbalance? I mean we've, we've talked a little bit about that earlier today, but from just your real life experience of patients, what have you seen kind of be triggers so to speak? Let's
First, first and foremost, um, I wanna address intermittent fasting. I think we made a joke about it earlier, but I do wanna, you know, speak to it because it's really popular right now. A lot of people are talking about it on social media. Um, intermittent fasting is really only studied in men currently. And we wanna be mindful as women with hormones that are different from men that intermittent fasting can actually be a little dangerous. Um, intermittent fasting can also put us into caloric restriction. And so these times without food are actually real stressors on the body. So we wanna make sure that our body feels safe and intermittent fasting can kind of hurt that. Um, so I do just, I wanna make sure everyone knows that <laugh>. Um, but yeah,
That was, no, that's really interesting because I to know that that research has only been done on men and of course men metabolize differently than a female body would. Um, and to be careful that you're not causing great dips, right. Highs and lows in the metallic, uh, metabolic system. Does that make sense? Absolutely. Clearly I'm not an expert on
This <laugh>. No, absolutely. And you, you want your body to feel safe, you wanna maintain, you know, you don't wanna feel stressed out because you haven't eaten in 18 hours. Cause we've all been hangry. We know what that feels like and that's not a, a good place to be.
Right, right. No, for sure. Um, and going, uh, going back to just curbing inflammation, um, how, is there some ways that, that we can look at our, our day and say, okay, what can I do that can help my body from going into these, these flares? We hear a lot about endo flares. What do you recommend? I
Can go, I think one thing that I see a lot with patients is working on making sure that people are matching exercise to their ability. I think a lot of my patients with endometriosis are like, oh, I should be doing CrossFit and running a marathon. It's like, I don't want you to should on yourself like that. You know, you want to kind of match like the inflammation that your body can handle from acute exercise with making sure that you're continuing to exercise because it's continuing to exercise will also reduce inflammation, help hormones generally. So exercise is really important, um, but you also don't want to be doing too much. So trying to find the line between too much and not enough is, is really hard and is something that you can work on with a physical therapist who really gets that. Um, and of course there's the whole dietary side to it, which I will not talk about <laugh>, but, uh, yeah, so
Exercise very important. Well, just to go about the exercise component, cuz we've, we're in a culture that's like, you go hard or you go home and it's like, uh, yeah, okay, well that kind of hurts a little too much and not in the right ways where it's serving me and I'm feeling like there's a good response. And there was a study I think that came out, uh, within the last month that, that a scientist said that running like hard long distance running is actually really counterintuitive to health and can cause a lot of joint issues. It could hurt even reproductive organs. So to hear about knowing what your body can handle and sometimes we don't know it until we've tried it. So is would you recommend, and from a PT standpoint, um, more gentle exercises like yoga, Pilates, stretching, walking?
Yeah, I mean, I think you just have to see how you're feeling also, you know, during certain parts of your cycle it's gonna be more optimal to do different kinds of exercises. So right before your period enduring, you may just wanna be, be doing gentle stretching and walking, but maybe right after your period you could try to do some more high intensity exercises. Um, you don't wanna be trying to do high intensity all the time. And yoga is wonderful because it really relaxes your pelvic floor and allows you to take nice deep diaphragmatic breaths. I mean, I think with endo, because there's so much pain, we're constantly holding our bodies so tight, like clenching, sucking in our stomach, but when everything's all sucked in, your pelvic floor muscles are tight and then it just kind of contributes to the pain cycle. So that's why yoga could be really helpful.
Yeah, I I also think it's important to really try to find the balance because I don't, I wouldn't say, oh, just doing yoga is maybe enough for everybody. It really depends on who you are and it really needs to be very individualized, I think. Like back to the point of everything's go, go, go. I think that that kind of culture of it is bad, but I think for on an individual level, you should be doing as most as you can. That isn't too much, but how do you know that, you know, it's, it's really hard to figure out. Um, but doing, I mean, cardiovascular exercise, there's good, um, evidence on improved cardiovascular fitness and overall pain and chronic pain. Um, and so increasing exercise is great, but then you also don't wanna do too much. And so I, I feel like especially in the, in light of that kind of go, go go culture we're talking about, I would make sure, I don't want people to do too much, but I also don't want people to like just do yoga. And I know that that doesn't help a room full of people <laugh>, but I think it's helpful to take that information and be like, okay, how can I figure out where my line is? And again, emphasizing what Cara said about, um, the cycle training, because that can be really important to push yourself when it's appropriate and then give yourself grace when it's appropriate. So it can kind of fluctuate, but,
And is that more of a trial and error kind of way to, to approach it? Because I mean, you can only really have yourself to figure out what works for you. So is it I'll try all these things and then see how my body responds?
Yeah, it can be done that way. Um, or you can work with either like a trainer that knows some of this stuff. I mean, I'm biased, work with a physical therapist, come to our office <laugh>. Um, but yeah, I mean it's, it's knowing yourself and knowing, like if you were to go try to do a 10 mile run, like you probably feel like trash and if you did like 30 seconds of stretching, like that's not gonna maybe be enough. So trying to work up slowly and gradually to find where the line is can be really great. Um, additionally like educating more on knowing what cycle training is that again, Cara talked about a little bit about what parts of your cycle you might be able to push yourself a little bit harder and what parts you might not be able to. Um, and again, that still has to be very individualized because what someone feels like on day one of their period is different from somebody else. And so, um, you kind of have to further individualize that. But general education on what parts of your cycle in theory should be more helpful versus not can be a great place to start. And then individualize from there.
From your experiences, um, N P T specializing with, with people with endometriosis, have you found certain exercises, certain, um, just regimens to be more helpful than others? And this is a very general question because we know it's so individualized.
I mean, I would say in general, most people are doing more yoga and some Pilates, um, they tend to do well with it paired with walking, you know, we obviously have people that like to run and do CrossFit and things like that. But I would say on the whole it's some, it's more gentle movement that seems to be more helpful.
And then with the, the food process. Yeah, which we've had a lot of conversation about the science of food and then of course you must have just loved that, right?
Oh my gosh, you're, I came in early just so I could see it and it was so worth it.
I could see your eyes are lighting up over that topic. So, um, so coming down to having, uh, a client who's saying, okay, I am not feeling well, I'm ingesting what I think is, you know, the right diet for me, how would you evaluate that person and try to figure out what could be causing inflammation or distress within their bodies from food?
Absolutely. So I mainly focus on the digestive system and really how we can affect, uh, proper digestion of food because that means, you know, less bloating, better nutrient absorption, more energy, you know, feeling better. So I like to take a top down approach and really I speak to my clients first and foremost about how are you eating your meals. Um, so I always like to look at like, are you sitting in front of the TV watching true crime? A lot of us do it
<laugh>
That sets off a stress response. So now you're eating your food in a stressful situation, no different than eating lunch at your desk or in the car or over a difficult conversation. So I wanna make sure your environment set up is calm, cool, collected, relaxed, because that way you're in that kind of rest and digest side of the nervous system. And then I really wanna make sure that you're chewing your food really, really well because when we chew our food, well we're increasing the surface area that's available for those, uh, enzymes to break it down. Better breakdown means better absorption means more nu more nutrients, your cells are gonna be a little bit happier. And then it also means less bloating and less constipation. So our collaboration really focuses a lot around constipation and chronic constipation. And so mealtime habits make a really big difference in that.
And then also with pt, talking about just the interdisciplinary approaches and kind of being a teammate on all of that, um, for constipation and bloating and all part of the inflammatory process. Are there certain exercises to kind of help move along the intestines manually? Because I've heard of the, is it the love method? Yeah,
Yeah, yeah. So there's the I L U massage, which is just a basic colon massage that you can do to yourself. Um, there's other stretches and exercises that will help relax the pelvic floor. And then the last piece is biofeedback, which is just, um, it's basically a way to figure out what you're doing with your pelvic floor muscles because what so often happens is, again, when your pelvic floor muscles get tight and you're going to have a bowel movement, you may be tightening them instead of relaxing them. So we can teach you how to relax them using a machine or we have other internal devices, but it's really important that you, you are actually relaxing your pelvic floor muscles when you're going to the bathroom so you can get everything out.
Yeah, I of course agree with that <laugh>, but I always explain this to my patients as like, you've never watched anybody else go to the bathroom. Like you have no idea if your defecation mechanics are like other people's or, or if they're the most optimal for you. Like if you didn't know how to do a squat, you could reasonably go to a gym and watch other people and like sort of figure it out. But you can't necessarily watch other people go to the bathroom and figure out how to improve your defecation mechanics. Mm-hmm. <affirmative>. And so that's kind of where we come in cuz we do know what proper defecation mechanics are and we can really help you through that in a way that's optimizing your system. Does everybody have perfect defecation mechanics outside of endometriosis? No. Um, but some people can get away with having less than optimal defecation mechanics when you had so much go on in this area and you struggle with constipation and all this stuff, you want to really hold your biomechanics and this defecation mechanics to the highest standards so that you can have as good bowel movements as possible.
So
That's a good one. And it, and it does have a lot to do with, like you said, the inflammatory processes and how your body's responding for simple things is like you should be keeping your feet flat when you're going to the bathroom, but Right. Is that, is that kind of right?
You want your knees above your hips? Okay.
Oh yeah. So stool you need like a stool need stool, you need a stool, you need a stool for the stool. I made a really bad poop joke, so there you go. <laugh> <laugh>. No, but there's, there's a lot kind of to align to make sure that your body, because when you do have endometriosis is so much more sensitive to all the processes and and to how things are relating. Um, I would because I feel like we, we don't get, there's so many questions out there so I'd love to just open up the floor if there's any questions.
Have Amanda in the back? No.
Um, as far as the exercise for someone who has blebs, um, that are caused from endometriosis on their lungs, should they not be kind of exercising? You say you could exercise a little bit more after your period or, but what about if you have the blebs on your lungs? Is that like, I don't know if that can affect that and make one burst or,
I
Don't know. I'm not, I don't know if I have a good answer for that. I mean, how do you feel after your period?
It's my
Daughter. Oh, your daughter, sorry. Okay. <laugh>.
Yeah, I mean I think of course in that kind of situation I would wanna double check with any referring physician or surgeon to make sure that like you're cleared to exercise. But from there, like they're still I think estrogen dependent tissue and so when you are in having symptom period symptoms, like they're gonna be worse. And so I think giving yourself that kind of grace during that time where they're more inflamed and then pushing a little bit more when they're less sensitive, um, I think would be a good way around that. But of course that goes back to what I was saying earlier about doing the most amount of exercise that doesn't like inflame you further or cause any kind of like discomfort. So it's again, has to be a very individualized approach.
Uh, I'm hearing a lot about constipation. Um, what about chronic diarrhea and how does that play into it? I know for most of my life, um, it was, I mostly suffered from chronic diarrhea and then random bouts of constipation. Like that was the combo, um, of my, like that was my overall, that's just how my bowel movements were all the time. Um, so yeah. So is that, is that a normal case? Do you see a lot of that as well? Was that, was I just a mystery in terms of that with the endometriosis or what
Are your thoughts? Yeah, so we see it all the time and sometimes what can happen is that if there is actually hard pieces of stool in the rectum, you can get this kind of like seep through diarrhea that comes around it. So sometimes the diarrhea can be a consequence of the constipation. So sometimes if you treat the constipation and get things out of the way, the diarrhea will clear up. Um, but I mean one of the biggest things with the diarrhea too is we wanna work on stool consistency. So probably Charlotte could help with that too. Um, just on the Bristol stool chart, you wanna keep it between a three or a four, which I'm sure you know already <laugh>, but sometimes actually the constipation, if you get things moving, it will help the diarrhea.
Yeah, and everything I said about defecation mechanics before still applies. Yeah. So yeah,
<laugh>.
Yeah, and food wise too, just always make sure you're avoiding any trigger foods and then really consider fiber. So consider how much fiber you're having, how many different types of plants you're having in a week. We also wanna look at your microbial balance in your microbiome, so we wanna make sure that, that it's all kind of coming together. So look at food diversity, different types of fibers, making sure you're hitting that like 35 grams of fiber in a day and um, and see how you feel. Also cooked foods are sometimes a lot better for diarrhea than, than the raw foods.
One more question
Over here. Um, you mentioned earlier that there's studies about the different color of foods and how some of them are more beneficial than others. Um, can you just elaborate a little more on what you guys are finding with that?
Absolutely. I actually have a printout of it in my bag so I can share it with you after. Um, but really what we're seeing is that all the colors have different benefits and they work synergistically. So you get the most benefit from eating as many different types of plants, but also all the colors of the rainbow. And this is like really on a daily basis, um, I know it seems very juvenile to say like eat the rainbow, but like really eat the rainbow because it's really good for you in that these, uh, these phytonutrients and these phytochemicals are helping to lower the inflammation in your body. Um, but they also act as food to those beneficial bacteria, like we said. So wide variety, enjoy all your fruits and veg, cook them if you're experiencing digestive issues because raw fruits and vegetables also can be tough to break down and just chew it really, really well. You're welcome.
Hi, uh, I am wondering
About, um, SIBO and also Immo. I was diagnosed with Immo twice and I've been really curious about how endometriosis might be connected to that. I know that like many of my clients and patients who have endo also have SIBO diagnosis or multiple sebo diagnoses. And so I'm curious yeah, what your thoughts are on like dietary interventions because I know obviously antibiotics, I, you know, I, I trust in my doctors and they tell me antibiotics are a good idea and also I think a lot of people probably would love to be doing anything we can preventatively to like keep our gut health in good condition.
Absolutely, absolutely. So SIBO is really tough and for those of you who don't know what SIBO is, it's small intestine bacterial overgrowth and it's where we get an overgrowth of bacteria in that small intestine where it's not supposed to be. Um, it can create a lot of bloating and gas and uh, acid reflux and a whole host of symptoms. Um, I like to kind of look at that one of the many root causes of cibo and um, sometimes it can be low stomach acid, so I wanna make sure that you're not getting acid reflux, also you're not feeling any sort of upper GI distress because it might mean that you don't have enough acid there to break down your food, but also to kill off the bacteria that are making their way into the small intestine. So, um, things that you can do is like, you can try a little bit of vinegar before meals, chew your food really, really well, and also eat in a relaxed state.
Cuz again, if we're not relaxed then we're not gonna make that stomach acid. Um, and then this, the antibiotics, they do work, I have clients all the time that have great results from the antibiotics, but I also have them come back in six months with the same symptoms. So I like to see like a combined approach where we do something like the antibiotics, but then you're also doing lots of different types of fibers and a really diverse, um, diet of different types of plants, um, with, you know, great stomach acid levels. So it's a really combined approach and it's also very individual to you. So those are just some of the things that I use, but you guys can maybe speak to the, uh,
Yeah. Um, sometimes too, it could be accompanied by, um, something called a domino phrenic dysuria, which is where your diaphragm in your abdominal muscles work the opposite of how they're supposed to. So as you're trying to digest your abdomen is actually contracting. So in physical therapy we can work on teaching you how to coordinate your breathing with your abdominal muscles, so it's not actually like pushing the contents of your stomach out. Um, and that it's kind of similar, similar to Endo belly because at the end of the day your stomach will be really protruded as opposed to in the morning it's totally flat. Thanks.
Yeah, and I think also what we were talking about earlier with that visceral mobilization is if you have a lot of either scar tissue or tension built up through your abdominal area, like everything doesn't have room to do what it needs to do. And so you wanna make sure that everything can like glide and slide over each other really well. So
Do we have any more questions? Oh, okay. Is the bacteria,
The bacteria that you're referring to, is that candida or is that way off track
<laugh>? Yeah, no, great question. The bacteria that I'm referring to are all the microbes that live in your large intestine, and this is what's considered our microbiome. And so we were talking about the, uh, the human genome project and talking about, you know, digestive health and these bacteria, they live there to further break down your food. They make a lot of immune cells. They play a huge role in, in health as a whole. Um, there can be candida in there. Um, we don't want it in high levels. And so that's where we would see something like a candida overgrowth, but that's what I was referring to
Adrian. Yeah.
Um, my question's more about pre and probiotics. So after my surgery I had infection and I was just put on high doses of antibiotics. So I was recommended to go on probiotics and recommend and probiotics. Is there such thing as too much probiotics or probiotics and like when to stop or how to like manage that?
Yeah, just like with anything, too much of a good thing can turn bad. So, um, I actually use like fermented foods and probiotics a lot of times with constipation because the side effect is bowel movements and sometimes if you go too far they can get really loose. Um, so that would be a side effect of having too much of a probiotic prebiotics. Those are the food for the bacteria. So if you give them too much food, a lot of times you're just gonna get a lot of gas, so you're gonna feel that bloating from too many prebiotics. So it is trial and error, but also look at food-based options as well. So like sauerkraut and kimchi are incredible options for fermented foods and for probiotics, um, mainly because, again, circling back to that diversity, um, you're getting upwards of 500 different strains of bacteria in just a tablespoon of kimchi. Whereas if you turn your probiotic pills over there might be five, maybe 10 strains maximum. So I like to use those foods because also too, it's really hard to eat a lot of kimchi or a lot of sauerkraut,
<laugh>,
<laugh>, I don't know, I I can't eat a lot of it. Um, and all those like fiber rich foods for your, uh, prebiotics.
Is there, um, is there, oh, sorry, yes,
There. Yes. Yeah. I think probiotics are something that should be consumed regularly, um, with or without antibiotics in your life. Um, we know that people who consume per fermented foods daily, more than one time a day, preferably like three times, um, have a much better functioning digestive system than those who don't. So all you really need is like a tablespoon of sauerkraut with each meal or a yogurt at breakfast, kimchi at lunch, sour crowded dinner, um, all that variety.
Awesome. Thank you guys so much. We're, uh, ready to kind of wrap up to the closing remarks now. So thank you guys. So
Excellent.