Bowel endometriosis refers to a condition in which the endometrial tissue grows on or inside the bowel walls, leading to painful bowel movements, constipation and diarrhea, and other gastrointestinal symptoms. The most common sites where the intestines are affected are, in order, the rectum, appendix, sigmoid, cecum, and distal ileum. If you experience symptoms such as IBS, leaky gut syndrome, or endo belly, especially in conjunction with painful menstruation, it may indicate bowel endometriosis flare-ups.
About Bowel Endometriosis
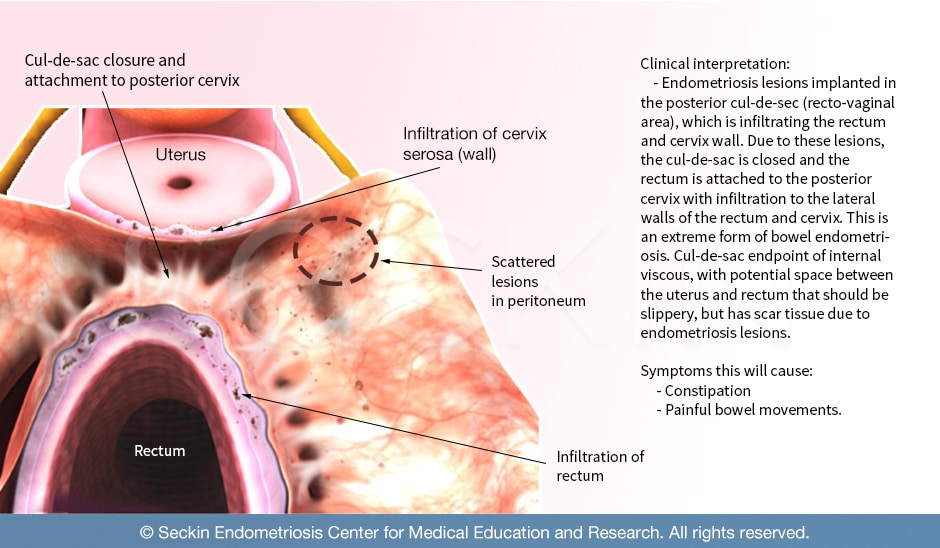
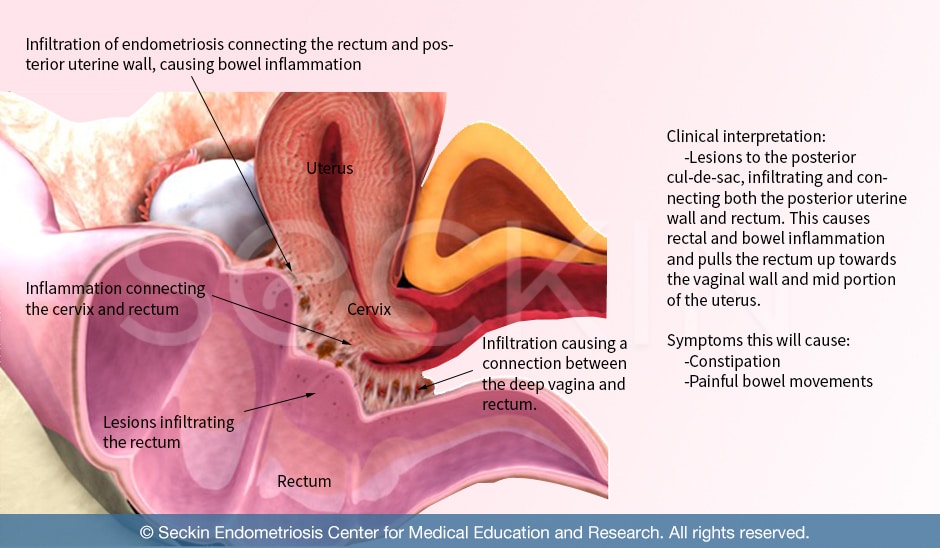
The severity of involvement is often limited to the serosal (outer) layer of the rectum and pararectal locations where inflammatory tissue hardened in the form of fibrosis. The most commonly affected portion of the bowel is in the cul-de-sac region and the anterior portion of the rectum, neighboring the upper part of the vagina. This area around the rectum, including the surface peritoneum is called the pouch of Douglas.
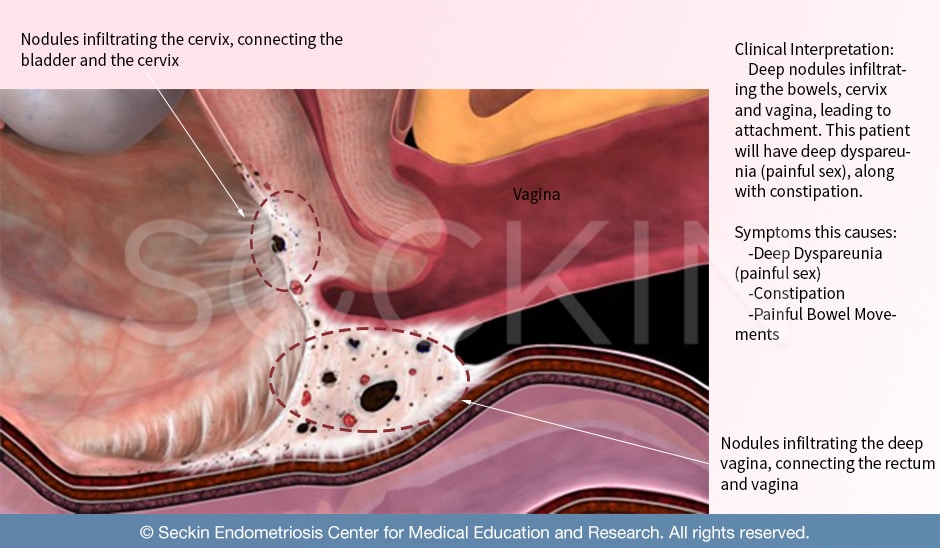
Peritoneal endometriosis in the pouch of Douglas is the most common but often overlooked type of endometriosis. If left untreated, the condition may progress and cause superficial and deep fibrosis, which can lead to scarring and closure of the recto-vaginal cul-de-sac. Persistent disease causing superficial and deep fibrosis is a common reason for dyspareunia, which refers to pain during sexual intercourse with deep penetration.
In peritoneal endometriosis, the tissue from the lining of the uterus attaches (implants) or regenerates (Stem Cells) in the peritoneum, leading to inflammation and causing significant harm to the healthy lining of the abdomen. The endometriosis lesions are usually found in multiple areas surrounded by peritoneal pores and texture irregularities. This leads to inflammation, stomach pain, and painful bowel movements. The bowel can be affected either at the outer serosal level or deeper within the tissue. Bowel and appendix involvement occurs in about 18% of all endometriosis cases.
The Surgical Treatment
The surgical treatment will consist of removing all of the peritoneal lesions by excisional technique with the purpose of borders free of disease. In deeply infiltrating endometriosis (DIE) the surgical approach may vary based on the involvement of the rectal wall and muscles. These are called shaving, nodulectomy, discoid resection, and finally anterior bowel, sigmoid, or ileocecal resection and end-to-end anastomosis.
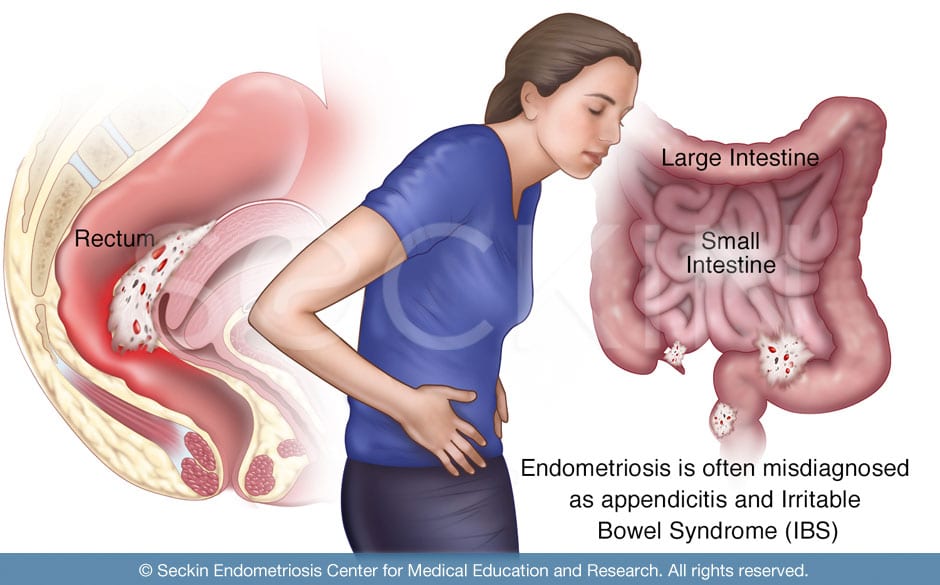
Endometriosis can spread to a variety of locations. It is common for patients to be unsatisfied with their endometriosis surgery when surgeons ignore their bowel symptoms and do not recognize their bowel lesions during surgery. Patients often receive a misdiagnosis of irritable bowel syndrome (IBS) or Crohn’s disease, as physicians mistakenly attribute their symptoms to a gastrointestinal cause. It is essential to ask whether or not a patient’s bowel symptoms are in sync with their menstrual cycle. If doctors do not ask these questions and do not alert the surgery team beforehand, the lesions will go unnoticed, unremoved, and untreated.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (212) 988-1444 or have your case reviewed by clicking here.
Facts about bowel endometriosis
Prevalence | 1 in 5 endometriosis cases infiltrate
|
Area of Involvement |
|
Difficulty Diagnosing |
|
Surgical Treatment |
|
Where does bowel endometriosis occur in the body?
In bowel endometriosis, lesions implant onto a multitude of areas outside the uterus.
- Peritoneum: This is arguably the most common site for endometriosis lesions. Peritoneal endometriosis has the same symptoms as bowel endometriosis. Therefore, it is important to evaluate the peritoneum in any endometriosis surgery, including bowel endometriosis.
- Cul-de-sac (pouch of Douglas): The area between the uterus and rectum, also known as the pouch of Douglas, is one of the most common sites of bowel endometriosis. In this area, the rectum and vagina face each other and are divided by the recto-vaginal septum. Endometriosis in the pouch of Douglas can cause painful bowel movements and painful sex as the inflamed affected tissue can infiltrate the outer wall of the vagina.
- Rectum: Endometriosis can implant onto the outside of the rectum, causing severely painful bowel movements, constipation, and rectal bleeding.
- Perirectal area: This is the area directly behind the rectum. Bowel endometriosis lesions that implant in this region cause back pain.
- Colon and small intestines: Lesions can attach anywhere on the outside of the intestines. This can often be tricky to spot. It requires a very skilled surgeon with a keen eye to inspect the intestines by “running” through them and checking for any lesions.
- Appendix: Often, lesions in the appendix or near the small intestine cause gas and pain on the right side (particularly the right lower quadrant).
What are the types of bowel endometriosis?
Overall, the lesions of the bowel can be multi-focal or multi-centered. Multi-focal means that lesions are in the same area, but there are multiple locations within that area of tissue. For example, there may be multiple lesions only in the rectum or upper vagina. Multi-centered lesions are also in the bowels but are spread diffusely throughout the rectum, colon, and appendix. In our own clinical setting, we have found that about 10-15% of our endometriosis cases have nodules that are multi-centered. In 20% of cases, the lesions are multi-focal.
Symptoms of bowel endometriosis
Symptoms experienced by patients with bowel endometriosis may be exactly the same as those associated with most bowel disorders. In fact, patients are commonly misdiagnosed with IBS, appendicitis, or Crohn’s disease.
To avoid misdiagnosis, it is important to distinguish the subtle—yet critical—differences between bowel endometriosis and other gastrointestinal diseases. If bowel symptoms worsen at different phases of the menstrual cycle, it is likely that the disease is endometriosis. For this reason, we encourage patients to record their symptoms throughout their menstrual cycle. Oftentimes, bowel dysfunction caused by bowel endometriosis will be in sync with a woman’s period, or at least alternate in severity during different points in her cycle. Women may receive many “normal” colonoscopies without doctors ever asking these questions. They almost always receive a “dump diagnosis” or “diagnosis of exclusion” such as IBS.
Symptoms of bowel endometriosis include:
- painful bowel movements, bowel spasms, and rectal pain, particularly increasing during periods
- bloody stools (while rare, this can be an indication of extensive endometriosis involvement)
- constipation, especially during periods
- diarrhea and constipation (some patients have diarrhea first then constipation, while others have the reverse)
- abnormal gas, especially during periods
- bloating (fluid congestion)
- abdominal tenderness, especially in the right lower quadrant due to possible appendix infiltration
- Painful sex (dyspareunia), due to infiltration of endometriosis to the rectum and posterior cul-de-sac of the uterus
Diagnosing bowel endometriosis
- Pelvic exam with sonogram: This clinical form of testing cannot provide a formal diagnosis of endometriosis. However, it can be helpful for your surgeon to assess points of tenderness. By performing a rectovaginal exam, an experienced surgeon can identify the specific locations of rectal tenderness. This coupled with sonographic imaging can provide a presumptive diagnosis as to whether or not the rectum and in turn, the bowels are involved.
- Imaging tests: Additional tests like an MRI and a dual contrast CT scan are necessary to evaluate the condition of the ureters, higher bowels, and appendix. The appendix is one of the first organs that, bowel endometriosis infiltrates. For this reason, it can be a key finding in presumptively diagnosing endometriosis before surgery.
- Laparoscopy: In order to formally diagnose and treat bowel endometriosis, laparoscopic surgery must be performed in the operating room. During this procedure, the surgeon makes small incisions into the abdomen. This allows them to insert operating instruments and a laparoscope (small camera). They then use this to visualize and evaluate the inner abdominal anatomy. Using this technique, a highly skilled surgeon can navigate through the bowels, which include the sigmoid colon, small intestines, and appendix, and thoroughly inspect them for any endometriosis lesions. They will then excise these lesions or completely resect parts of the bowels depending on the severity of the disease. They perform all of this under laparoscopic visualization, ensuring minimal invasive surgery and optimal recovery.
Why is bowel endometriosis often misdiagnosed?
Bowel symptoms are some of the most prominent endometriosis symptoms, even in adolescents. Endometriosis symptoms will often start with bowel symptoms (diarrhea, constipation, etc.), causing patients to seek a gastroenterologist, who will likely attribute the symptoms to IBS, appendicitis, Crohn’s disease, or even colon cancer.
These diagnoses are made without biopsy samples or a pathology report. Instead, patients go on to receive multiple colonoscopies and endoscopies and are often diagnosed without a full evaluation of what may really be the underlying cause of their symptoms. For these reasons, we consider an IBS diagnosis without evaluation for endometriosis a “dump diagnosis” for a patient’s bowel dysfunction and pain, particularly if they have symptoms that coincide with their period. Patients who receive such a misdiagnosis also receive the wrong treatment and experience persistent symptoms, only to find out, years later, that they had endometriosis all along. In some instances, patients can go five to 10 years without treatment, sometimes missing the prime reproductive years of their life.
Why can a colonoscopy not diagnose bowel endometriosis?
Whereas inflammation of the bowel caused by IBS materializes exclusively within the intestines. Inflammation caused by bowel endometriosis occurs when lesions attach to the outside of the bowels. Procedures such as colonoscopies and endoscopies can only examine the inside of the bowels. They are, therefore, unable to identify inflammation caused by endometriosis. Laparoscopic surgery is the only way to formally and definitively diagnose bowel endometriosis.
Treatment of bowel endometriosis
Surgical treatment
When a surgeon looks into the abdomen using laparoscopy, one of the first steps of the procedure should be to evaluate the appendix and ileum of the small intestine.
The surgeon will then perform a procedure called, “running the bowels”. This is when they run through all of the small intestines, like unwinding a fish hook, all the way to the stomach, and check for any lesions or deformities. They will then also check the diaphragm and colon (large intestine). In cases of redundant colon, which is an abnormally long large intestine that causes the widening of the intestine right before the rectum. This “running” procedure is particularly important as the sigmoid (S-shaped extra colon) must be mobilized completely. It is important to note that this technique takes great skill, and is part of the reason why bowel endometriosis cases are so complicated and present more risk. Therefore, only those with vast experience should perform this procedure.
Once the surgeon unwinds and frees the intestines. The doctor puts a rectal probe with a manipulator in order to perform a thorough examination of the rectum and associated rectal vaginal symptoms. And will then be able to check the bowels for suspected lesions and remove them accordingly, using their preferred technique. The treatments for bowel endometriosis are either the removal of the nodule(s), most of the time including the full thickness of the wall. If the nodules are multiple and obstructive, bowel resection surgery. This is particularly difficult and requires special skills in colorectal surgery.
Will a hysterectomy treat bowel endometriosis?
Advanced cases of bowel endometriosis may benefit significantly from definitive surgery. This would consist of a hysterectomy and a deep cleaning of the bowel endometriosis. However, 80% of cases do not require large-scale bowel resection surgeries. Instead, lesions are excised and the bowels repaired by sewing or suturing. This requires the special technique of suturing in “layers”.
A hysterectomy is only necessary in the case of end-stage endometriosis or if patients prefer to eliminate their fertility. Hysterectomies are often mistakenly viewed as curative surgical treatment for patients with endometriosis. Removal of the uterus eliminates menstruation but it does not treat endometriosis that has already grown and infiltrated surrounding organs. These lesions, if left untreated, may grow further, causing bowel symptoms to persist even after a hysterectomy.
When choosing a doctor, it is important to keep in mind that the doctor should not only check for endometriosis in the bowels but must also be qualified to remove lesions, even when the treatment plan involves a hysterectomy.
What is the recovery time after bowel endometriosis surgery?
In general, as long as the operation is performed laparoscopically, as is the case with all our surgeries, the recovery time is no different than any other standard laparoscopy procedure, and we discharge patients on the day of their surgery. However, for patients who undergo suturing of the bowels (conservative surgery), we advise an overnight stay in the hospital until they pass gas and have their first bowel movement. It is important to note, however, that bowel endometriosis surgery is one of the most difficult and specialized forms of surgery. So, complications can often arise. In fact, even with the most precise, skillful surgery, one in 20 bowel endometriosis cases presents some form of perioperative complication.
What to expect the days after the surgery?
Following bowel endometriosis surgery, you can expect your bowels to be very sensitive. You may need a few days to rest before resuming normal function. Below are just a few of the common complications that may arise for a few days following bowel endometriosis surgery, along with suggestions to help relieve these symptoms.
- Bloatedness causing back and shoulder soreness: Back pain is a common complication that can arise temporarily following bowel endometriosis surgery. Lesion removal, or simply bloatedness can cause this. During bowel endometriosis surgery, your abdomen will be filled with gas in order to lift the abdominal walls away from the cavity to get a better view of the bowels. After surgery, some of this gas will remain, but there are some remedies for relieving this.
- Abnormal and painful bowel movement: The first bowel movement following bowel endometriosis surgery can often cause pain and discomfort. While some physicians recommend the use of narcotic pain medications in these instances, we have found that narcotics cause constipation. We instead advise drinking at least 64 ounces of water a day and sometimes even a mild stool softener, such as Colace, if needed. We also recommend keeping your diet light for the first few days to give your body the time it needs to recover. This could include broths, jell-O, and other easily digested food.
What are the risks of bowel endometriosis surgery?
Bowel endometriosis surgery is one of the most difficult procedures to perform. It requires great experience and meticulous attention to detail, as a surgeon must go through the entirety of the intestines, from the rectum to the small intestines. For these reasons, bowel endometriosis surgery is the riskiest of any other endometriosis surgery. In our experience, nearly one out of 20 cases (5%) experienced complications following surgery, including bloatedness, gassiness, and abdominal and rectal pain. While this is a very promising recovery number for a procedure that only a select few can perform. We feel it is very important for the patient to be aware of the potential risks.
Can diet relieve the symptoms of bowel endometriosis after surgery?
Diet and lifestyle changes can be complementary measures in the treatment of bowel endometriosis, particularly before and after surgery. Endometriosis causes widespread inflammation leading to constipation, diarrhea, abnormal gas, and bloating. Therefore, patients may experience some symptom relief if they consume an anti-inflammatory diet.
What diet can help relieve bowel endometriosis symptoms?
There are many diets that may help. However, it is important to understand that every patient is unique and will respond differently. There is no one diet for endometriosis. Consulting with your doctor or nutritionist when making a dietary change and recording the effects of dietary changes on your symptoms may be useful in determining a diet that is appropriate for you.
One study found that a low FODMAP diet can be highly beneficial in relieving the symptoms of bowel dysfunction in endometriosis patients. FODMAP is an acronym for “fermentable oligosaccharides, disaccharides and monosaccharides, and polyols”. Some human GI tracts poorly absorb foods containing these molecules – mainly carbohydrates, with the exception of polyols (alcohol). Generally, a low FODMAP diet consists of low carbohydrates and gluten in order to reduce inflammation. Sugar and carbohydrates are harmful in many conditions including endometriosis, inflammatory diseases, auto-immune diseases, bacterial and yeast infections, and cancer. Sugar nourishes these conditions and worsens their associated symptoms. In the case of bacteria or yeast infections, it worsens the infection itself.
High and low FODMAP foods
| Food Category | High FODMAP foods | Low FODMAP food alternatives |
| Vegetables | Asparagus, artichokes, onions(all), leek bulb, garlic, legumes/pulses, sugar snap peas, onion and garlic salts, beetroot, Savoy cabbage, celery, sweet corn | Alfalfa, bean sprouts, green beans, bok choy, capsicum (bell pepper), carrot, chives, fresh herbs, choy sum, cucumber, lettuce, tomato, zucchini |
| Fruits | Apples, pears, mango, nashi pears, watermelon, nectarines, peaches, plums | Banana, orange, mandarin, grapes, melon |
| Milk and dairy | Cow’s milk, yogurt, soft cheese, cream, custard, ice cream | Lactose-free milk, lactose-free yogurts, hard cheese |
| Protein sources | Legumes/pulses, red meat | Meats, fish, chicken, tofu, tempeh |
| Breads and cereal | Rye, wheat-containing bread, wheat-based cereals with dried fruit, wheat pasta | Gluten-free bread and sourdough bread, rice bubbles, oats, gluten-free pasta, rice, quinoa |
| Biscuits (cookies) and snacks | Rye crackers, wheat-based biscuits | Gluten-free biscuits, rice cakes, corn thins |
| Nuts and seeds | Cashews, pistachios | Almonds (<10 nuts), pumpkin seeds |
Our approach
About one in four of our endometriosis cases involve the bowels. This is a bit higher than the normal number of bowel endometriosis cases in the average endometriosis patient. For this reason, we take both great pride and care in surgically treating bowel endometriosis. Having practiced our endometriosis laparoscopic surgery technique for several decades. Our team has great skill in handling even the most complex cases of bowel endometriosis with minimally invasive techniques.
Running the bowels
Once we make incisions into the abdomen and insert a laparoscope, we first check the appendix and ileum of the small intestine, as these are common sites in which bowel endometriosis lesions often implant. We then meticulously and thoroughly unwind the intestines (run the bowels) and insert a rectal probe with a manipulator. This mobilizes the intestines, making them accessible to examine and operate on. Then, we identify and remove suspected endometriosis lesions.
Repairing the bowels
A good surgeon must have a tremendous amount of experience in repairing the bowels, rectum, and sigmoid colon. This is arguably the most difficult part of bowel endometriosis surgery.
Many endometriosis lesions are difficult to remove without cutting into the mucosa, especially when the lesions are at the muscular level. In other words, these nodules are transmural with full-thickness involvement (buried within the muscular tissue), and will thus require distortion of the normal bowel anatomy so that the lesions can be removed. This will then require anatomical repair.

Over the years, we have mastered the technique of proper restoration of the bowels’ original function following lesion removal. We perform all necessary restoration, reconstruction, and repair of the organs that have been operated on. We then test the function of the intestines using an “air leak” test (or flat tire test). During this technique, we submerge the bowels in water and methylene blue dye. Then, we apply pressure to the area to push air into the intestine and ensure there is no leakage of the newly restored organs and the sutures are properly intact.
More complex cases
Sometimes, more extensive bowel surgery is necessary. When an infected organ or area of tissue is diffusely involved, segmental resection and anastomosis may be necessary. This is a procedure we use to cut into the bowel to remove areas of diffuse endometriosis. We then reattach the bowels to their newly restored anatomy. Other versions of this include serosal/peritoneum excision, nodulectomy, and disk and segmental excision. At times we may even end up doing multi-centered surgery, which involves rectal resection, sigmoid resection, ileocecal resection, and anastomosis. So, we can end up using three different resection techniques with anastomosis in order to thoroughly treat the multiple organ involvement that bowel endometriosis can cause.
What is our method of “team surgery?”
Endometriosis is a multiple-organ disease. This means that it can affect organs such as the bowels, bladder, diaphragm, and even the lungs and kidneys. For this reason, teamwork is a necessary component of our approach. Bowel endometriosis is particularly complex and requires a multidisciplinary surgical team to provide the best quality care to our patients. During these surgeries, Dr. Seckin and the teamwork with a team of highly skilled laparoscopic surgeons. The colorectal and urology specialists on our team have worked with us for many years. They have extensive experience in performing surgeries alongside Dr. Seckin. Our philosophy of endometriosis team practice ensures a high surgical volume of diversification and knowledge. This is crucial to minimize postoperative complications and increase the opportunity for a successful outcome.
How do we ensure a thorough bowel endometriosis surgery?
We strongly believe in increasing the quality of endometriosis surgery by removing endometriosis from every anatomical location including the bowel, bladder, nerves, and ureters. Many surgeons strictly focus on the reproductive system in cases of endometriosis. However, we believe in conducting a thorough examination of the abdominal anatomy in its entirety, which includes the bowels. A margin-free, complete excision without leaving any disease behind is the gold standard that our team practices. It is also important to not leave behind any scar tissue. This way the patient has a higher chance of recovery and symptom relief. There are also several key components and ideals we uphold in all of our endometriosis surgeries, in order to give the patient the best quality of care that they deserve.
Our main components
Deep excision:
One of the main reasons excision surgery is the preferred method of lesion removal is that it removes each lesion in its entirety. Methods of fulguration and laser ablation present a risk of harming surrounding healthy tissue. They also only remove lesions superficially. This increases a patient’s risk of symptom recurrence. “Deep excision” removes each lesion out of the tissue’s entirety while preserving the borders of the surrounding healthy tissue.
Cold excision:
Techniques of laser ablation and fulguration often rely on heat and electricity to destroy lesions. These are often unnecessary uses of powerful energy sources that damage the surrounding healthy tissue, while only removing lesions superficially. This is why we thoroughly believe in “cold excision,” or excision surgery that stresses the use of minimal to no electricity.
Pathology report:
Using excision surgery, we are able to preserve removed lesions. Then we send them to a pathology lab, where a pathologist examines them under a microscope. This is a crucial component of our surgeries, as it is the best way to formally diagnose endometriosis. It also allows us to gain a better understanding of its possible spread and growth. Many other surgical methods are unable to generate a pathology report as they destroy the endometriosis tissue.
Minimally invasive surgery:
We ensure our patients that our surgeries, even those as complex and thorough as bowel endometriosis excision surgery’ are performed with the most comprehensive care, ensuring minimal invasion and the best chance of symptom relief and recovery.
Experience and skill:
At the Seckin Endometriosis Center (SEC), we have been training for decades to surgically treat different types of endometriosis cases through laparoscopy. Bowel endometriosis is no exception. Over time, we have gathered the skill and knowledge that is necessary for complex treatment options such as surgical excision of bowel endometriosis.
The result
Bowel endometriosis surgeries require a surgeon to complete meticulously demanding tasks such as running the entirety of the intestines to inspect for endometriosis lesions and reconstructing, repairing, and restoring the bowels after they have been operated on. We have learned that such surgery does not only require great experience but also calls for keen attention to detail. Only through meticulous surgical execution can a surgeon remove endometriosis from the bowels. By removing these lesions, we provide our patients with the highest chance of recovery and symptom relief.
Patient story
Bowel endometriosis usually occurs in less than 20% of all endometriosis cases. However, in our practice, nearly one in every four patients show signs of possible bowel endometriosis. We have a number of bowel endometriosis stories from patients who underwent bowel excision and resection surgery.
Meet Patrice M. She was rushed to the ER due to an ovarian cyst bursting in her right ovary, only to find that her endometriosis had spread to her bowels. Read more stories of patients who had endometriosis surgery after their disease spread to the bowels in our testimony section.
Get a Second Opinion
Our endometriosis specialists are dedicated to providing patients with expert care. Whether you have been diagnosed or are looking to find a doctor, they are ready to help.Our office is located on 872 Fifth Avenue New York, NY 10065.
You may call us at (646) 960-3080 or have your case reviewed by clicking here.
Dr. Seckin is an endometriosis specialist and women’s reproductive health advocate. He has been in private practice for over 30 years at Lenox Hill Hospital with a team of highly skilled personnel.
Dr. Seckin specializes in advanced laparoscopic procedures and is recognized for his expertise in complex cases of deep infiltrating endometriosis of the pelvis. He is particularly dedicated to performing fertility-preserving surgeries on cases involving the ovaries.
He has developed patented surgical techniques, most notably the “Aqua Blue Excision” technique for a better visualization of endometriosis lesions. His surgical techniques are based on precision and microsurgery, emphasizing organ and fertility preservation, and adhesion and pain prevention.
Dr. Seckin is considered a pioneer and advocate in the field of endometriosis.

